Dr. Augustine M.K. Choi, the Stephen and Suzanne Weiss Dean of Weill Cornell Medicine and provost for medical affairs of Cornell University, plans to return to his research at the end of the calendar year, following his tenure as dean. We sat down with Dr. Choi to discuss the ways the institution had evolved under his six years of leadership.
This interview has been edited for length and clarity.
Weill Cornell Medicine: When you consider where we were in 2016, what strikes you most about the institution's growth and change?
Dr. Augustine M.K. Choi: We have incredible momentum in our tripartite mission: to care, discover and teach. Our clinical operations, led by our physician organization, are as strong as ever, despite the challenges presented by the pandemic. Our educational mission continues to be exceptional, recruiting the brightest students to become the best doctors and scientists they can be, thanks to our momentous debt relief scholarship program. And then, of course, our research - the cornerstone of our We’re Changing Medicine campaign and the sustained growth in NIH funding over the last five years. The strong momentum and the tailwind we have behind us bodes well for years to come.

Dean Choi announcing Weill Cornell Medicine’s new scholarship program at an event on Sept. 16, 2019. Credit: StudioBrooke
WCM: Speaking of our scholarship program, how did its expansion in 2019 change the way we provide medical education? How did it impact our students?
AMKC: There are two key reasons we did it. One, of course, is equity for all students. It's a very expensive process to apply to medical school – the application, the interviews to get in – and to become a doctor. We needed to send a strong message to anyone in the U.S. that if you want to be a doctor and you can't afford to apply to a school like Weill Cornell Medicine, but you qualify for financial aid, you can graduate without the burden of substantial student loans.
And the second reason we did it, also related to equity, is the average debt of a student in the U.S. was just very daunting – nearly $200,000 in average debt for private school education. We did not want to burden students with that type of financial threat, which adds to burnout and compromises their wellbeing. That financial burden would affect them after they graduate as physicians.
The early numbers show that the program has made a tremendous impact on first-generation college students. Our enrollment numbers for underrepresented groups were always strong, but now they’re even better. We are now consistently in the high 20 percent range, with more applications from public universities rather than private. So, in all metrics that we look at, the trend is going the right direction and really fulfilling the objective of our expanded scholarship program, which was to have everyone have a fair shot and achieving equity among our students.
WCM: Over the last five years we've seen enrollment increase by about 24 percent, driven in large part by new master's degree programs in the Weill Cornell Graduate School of Medical Sciences. We've also had programs expand in geographic footprint, including a Ph.D. program at Houston Methodist. What does the growth of our educational programming say about how we're training the next generation of leaders in science?
AMKC: Our master's programs have expanded from one program to seven by emphasizing innovation in higher education. If you just had growth in the number of students in one particular program, that's good, but that's just volume. What we have is expansion and innovation. The newest program is in biomedical imaging, for example, and will be highly sought after. Master's programs attract different types of career phenotypes, and that’s especially true with this program. There's a strong need for expertise beyond undergraduate training by really specializing with a master's in imaging modalities.
Every medical school has a different vision and they are all noble. Like many of our peers, our main mission is to train the best physicians and physician-scientists to become leaders no matter what area, whether it's clinical, research or administration. Research is a principal component of academic medicine. Every year, the Association of American Medical Colleges releases data on 10-year student outcomes. Last year’s data showed 43 percent of our graduates are now in full-time academics. The national median is 27 percent. That's a big, big gap. Ever since I became dean, our number has always been in the top tier.

Dean Choi filming during the 2020 virtual commencement ceremony. Credit: StudioBrooke
Our success reflects our mission, the quality of our faculty and mentors, and what type of curriculum we have. We went to a new curriculum about eight years ago that is propelling our students and preparing them very well to enter academic medicine.
There’s also our Tri-Institutional M.D.-Ph.D. program, now in its 50th year, and we're very proud of that. Rockefeller has its own tremendous strengths as a unique graduate school. Memorial Sloan Kettering is the biggest cancer center. Our three institutions have important synergies that bolster the kind of education we provide together.
WCM: We've placed a strong emphasis on student wellness over the last five years. We doubled the amount of dedicated space for study and recreation through the Feil Family Student Center and the Lasdon student area. We're building a state-of-the-art residence hall a few blocks from campus. We hosted the first-of-its-kind National Conference on Medical Student Mental Health and Wellbeing in 2019. Why is it so important to support the mental health and wellbeing of our students? How does this affect their future success as health care professionals?
AMKC: Wellbeing is essential – not just for our students, obviously, but for the community at-large. We all know that the most effective doctors are those with physical and mental health strength. If you yourself are not in top shape physically or mentally, it affects your work. It’s no different than a professional athlete.
In the goal of providing excellence in patient care, you need to provide a training environment with an effective learning experience. That’s curriculum, living space, student centers – all the things you mentioned. And soon, thanks to our campaign, better housing.
We had a terrific national conference on student mental health. Supporting physician wellbeing and protecting students from burnout have been important concepts for years, but haven't been prioritized until recently. When I was going through training as a medical student, the emphasis on this need was not as obvious as it is now. Weill Cornell Medicine took the lead and we’ve made tremendous progress.
WCM: Our sponsored research portfolio has increased nearly 50 percent over the last five years. How does this growth and funding support impact the scientific landscape at Weill Cornell Medicine?
AMKC: Research is an area, just like clinical care, where you need to continue to advance and grow, because science itself evolves. What we knew 200 years ago, 100 years ago, 10 years ago is very different than what we know now because of the inherent nature of what science is. We have to continue to push the needle in discoveries, and it is why we are very proud of our success in growing the research enterprise.
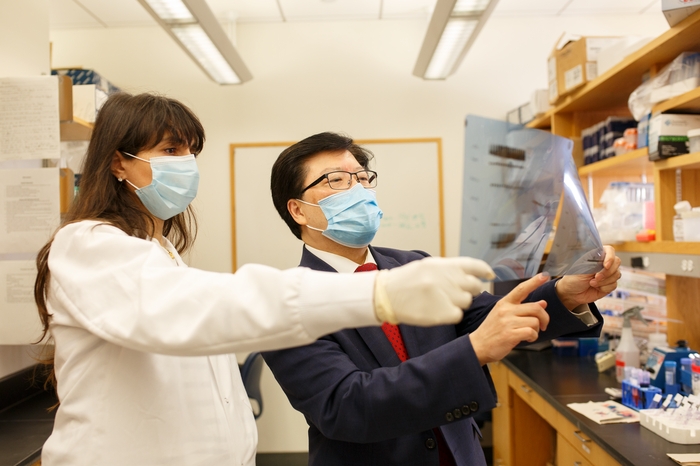
Dean Choi in a pulmonology laboratory. Credit: Julia Xanthos Liddy
It is also critical to attract the best trainees, whether they're students or postdocs. When you're a trainee, you want to join a laboratory that is exciting, making innovative discoveries and to be a part of the conversation. And at the end of the day, we hope our discoveries have an impact on clinical disease, patient care and, ultimately, human health.
Research and development starts in academic laboratories, and we need both to continue. This is why we need to be aggressive with capital investment in research space to continue the momentum.
WCM: We've established several multidisciplinary research centers and institutes that transcend traditional academic departmental structures. How does this kind of arrangement and collaboration help foster scientific curiosity and creativity?
AMKC: We are now squarely in the era of team science. Early in my career there was team science but it was all siloed between the bench people and clinical research people. Now, with so many advancements, the fields are getting very blurred: basic to translational, translational to clinical research, clinical research to clinical trials.
You need basic scientists -- people to make the discoveries and translate that to humans. And then you need a variety of disciplines – genomics, bioinformatics, now data science and artificial intelligence – to make the translation of the discovery to patient impact.
Team science is essential and here to stay, and this is one of the major reasons we set up the translational centers in the Belfer Research Building. I think that's going to be a major part of the equation in our scientific endeavors to better understand disease and come up with new diagnostics and therapeutics.
WCM: Many of our advances in the clinical enterprise over the last five years came through our deep collaboration with NewYork-Presbyterian. Those include the opening of the David H. Koch Center, unification and integration of electronic health records through Epic Together and expansion of care offerings in Brooklyn, Lower Manhattan, Long Island City and Southampton. How would you describe the partnership with NYP?
AMKC: Both of our institutions together make this medical center the best it can be. I’m very proud of our collaboration and accomplishments. After a decade at Weill Cornell Medicine in various leadership positions, I’ve learned our success and NewYork-Presbyterian's success are mutually beneficial; we need each other. That’s a credit to the leadership and the Weill Cornell Medicine Board of Fellows and the NewYork-Presbyterian Board of Trustees. Steve Corwin’s leadership has been stupendous.

Dean Choi at the 2017 wall-breaking for the Feil Family Student Center, along with (from left) Dr. Barbara Hempstead, Jeffrey Feil and his grandson Tyler Lincoln, and Jessica M. Bibliowicz.
We have done some great things together, not only the everyday patient care that we jointly deliver, but also the formal collaborations that really move the needle. WCINYP [Weill Cornell Imaging at NewYork-Presbyterian] is an excellent example of providing optimal patient care, while being fiscally efficient.
Our Accountable Care Organization (ACO), which also includes Columbia, has been credited by Medicare and we’re getting money back in savings for the last three years. Last year we had more Medicare savings than any other area ACO in our area.
Our shared patient database, Epic, has created efficiencies. We contributed immensely because we were the first ones in our system to implement it 25 years ago. When NYP wanted to move to Epic, we did it together – NYP, Columbia and us.
NYP is also helping drive innovation. There is no doubt that they are technologically one of the most innovative health care systems – just look at what we’ve done together with telemedicine. In recent years, they really want to push AI in cardiovascular care and other areas.
WCM: The COVID-19 pandemic was a once-a-century challenge that required every part of the institution to rapidly adapt and react to a life-threatening disease. How do you think the pandemic affected the institution's culture?
AMKC: The way we got hit overnight - remember, March 1 was the first indexed case in New York, and on March 15 we had 300 patients in the hospital and all ICU beds were COVID. That tsunami in those three weeks was a jolt that no other medical center experienced. The pandemic united us to fight this coronavirus to save lives. There’s a fight or flight physiological response to danger - and COVID unearthed all of our abilities to adapt. We needed strength, innovation and the DNA of both NewYork-Presbyterian and Weill Cornell Medicine to really combat this coronavirus virus physically, mentally, emotionally and financially.
At the end of the day, it changed the landscape of health care.
WCM: We’ve had a longstanding and distinguished reputation as a champion for diversity and inclusion in science and medicine: from our pipeline programs and the creation and growth of our annual Diversity Week to the elevation of a senior associate dean for diversity and inclusion, the establishment of the Office of Institutional Equity. Can you speak about the importance of all the efforts in diversity and how it's enhanced our institution?
AMKC: If you look at our growth in research in dollars and principal investigators, if you look at growth in clinical receipts and even growth of our students, it is part of the culture but it doesn't necessarily enhance the culture. How do you enhance your culture?
This is where your intangibles and core values as an institution count. They are no different than core values of a human being, which are fairness, justice, respect and equity. As an institution, we are very proud that we are part of an “any person, any study” university. In 1898, we were one of the few medical schools in the country that even accepted female medical students.
The pipeline programs that evolved over years, those didn't happen overnight. All the pipeline programs that you know of – Travelers, Gateways, WISER – I mean, we have just about every segment of our students and the pipeline programs covered. That doesn't solve all the problems of equity among students, but it's a great start and the yield is quite good. We have really tried in earnest to focus on diverse faculty recruitment.
When it comes to equity and justice, there's no end to it. The sky's the limit. As we continue to push the needle, it will continue to enhance our culture. And that itself is so powerful because institutional cultures don't come and go. Cultures stay. We’re very proud of what we have done, but we are just trying to contribute to this big space as much as we can as an institution.
WCM: What influence have you seen our work in diversity have on other academic medical institutions?
AMKC: Humbly, they have come to us. I have been invited to more than 10 universities and medical centers to talk about equity and our initiatives. I get calls and emails from people coming from places with robust programs. They were just amazed by what we are doing here. This is an area that you don't want to put up your pamphlets and signs of how great we are; we just did the work. We were recently recognized five years in a row for the Higher Education Excellence in Diversity awards, which is a tremendous honor. But being recognized by our peer institutions, leaders and faculty across the nation is significant and important to me.
Your approach cannot be drip, drip, drip when you're trying to lead. That doesn't work. The effort has to be with the same force as an open fire hydrant. We've done that.
WCM: The institution has also prioritized mentorship as an essential pillar for career advancement. How does new institutional infrastructure, a new senior associate dean for faculty and programs like the Jumpstart Career Development Awards, support these efforts and why is mentorship important?
AMKC: Mentoring is one of the essences of a life of vitality, along with equity and wellbeing. And mentoring, if you look at our Office of Faculty, we didn't even have that office four years, five years ago, so we established it. Their charge isn’t about pushing promotions or checking off the boxes; it’s evolving into an office of mentoring.
Now at our institution, almost every academic department has a robust mentoring program that did not exist just five years ago. Mentoring is such a big part of the everyday language and that's what you need. It’s not how many dollars or how many grants; it's the culture of the mentorship near you that is important. And I'm seeing that at every corner that I turn.
WCM: We have global health roots tracing back to Ida Scudder, who was a pioneering physician in India and alumna at the turn of the 20th century. Today we have robust clinical research and education programs on five continents, and a new Office of International Affairs to support them. What do our global partnerships mean in a post-pandemic world?
AMKC: It's part of our special sauce at Weill Cornell Medicine to have a global footprint. Team science, collaboration, equity and diversity all have an impact on patients. And what better way to do it not just in the North American continent but in Qatar, in Salzburg, Eastern bloc European countries, Haiti, Tanzania and India.
Our physician-scientists around the world represent the core values of Weill Cornell Medicine. What Dr. Bill Pape is doing in Haiti at GHESKIO, what Dr. Rob Peck and folks in Tanzania at Weill Bugando are doing, what our faculty are doing when they go to Salzburg to teach at the Open Medical Institute, what Weill Cornell Medicine-Qatar is doing with training the best students. It just keeps expanding outside New York City and collectively reflects all the things we've talked about. It's a big window to our DNA, if you think about it.
Dr. Steven J. Corwin and Dean Choi at the We're Changing Medicine campaign launch on June 17, 2021. Credit: StudioBrooke
WCM: In 2021, the institution publicly launched its $1.5 billion We're Changing Medicine campaign, inspiring our community of students, faculty, staff, donors and alumni to help us change the future of medicine. We just passed the halfway mark of that eight-year campaign and are on the cusp of having raised $1 billion. Why do you think our vision is resonating with our donors?
AMKC: Well, it's resonating because the core values of our campaign match the core values of our great board members who care about society. They all have their personalized areas of interest, whether it's research or in research of cancer or neuroscience, or education and scholarships. They share the core values of Weill Cornell Medicine and what it stands for. They don't have to say it. I can feel it, I can hear it, I can palpate it.
It comes down to providing world-class treatments with the most compassionate and humane care. We are driven toward excellence and innovation in research to have impact on human disease and benefits for our patients. And of course, training the doctors and scientists to be future health care leaders.
This resonates with our donors. And is why we have raised almost $1 billion four years into our eight-year campaign. We are so fortunate to have committed board members and donors like we do. And I see nothing stopping that momentum. Nothing.

