A new technology developed by Weill Cornell Medicine and Max Planck Institute for Medical Research scientists allows the controlled, on-and-off “switching” of neural receptors with unprecedented efficiency and precision. The technology is likely to be widely adopted for studying these receptors and their links to behavior, and potentially will enable the development of better drugs for treating depression, schizophrenia and other brain disorders.
In their study, published on November 26 in Neuron, the scientists showed that they could attach a synthetically engineered, light-sensitive molecule to receptors of a chosen type, employing the molecule to turn neuronal signaling on and off with high efficiency. Among their demonstrations of the technology’s utility, the scientists used it to identify a precise subset of neurons in the brain where certain drugs to treat schizophrenia have their main effect.
The receptors the scientists rendered “photoswitchable” with their technology belong to the large family known as G-protein-coupled receptors (GPCRs), and the technology can now be extended relatively easily to other members of that family.
“We now have a general framework for being able to control GPCRs efficiently in living animals, and one of the reasons that’s important is that most drugs for treating neuropsychiatric disorders target GPCRs,” said co-senior author Dr. Joshua Levitz, an assistant professor of biochemistry at Weill Cornell Medicine.
Traditionally, studying the precise workings of GPCRs has been difficult. Even for a single type of GPCR, such as a receptor for glutamate—one of the principal neurotransmitters that mediate synaptic transmission—there are usually many different receptor subtypes that are distributed on different populations of cells throughout the brain. These subtly distinct receptors may respond differently to the activating molecule, known as a ligand, and also affect different brain circuits. That complicates the work of scientists who are trying to understand with precision how signaling molecules within the brain control behavior. It also complicates the development of new drugs, and even hinders the understanding of how existing drugs work and why they have certain side effects.
About four years ago, Dr. Levitz and co-senior author Dr. Johannes Broichhagen, who is currently a departmental group leader at the Max Planck Institute for Medical Research in Heidelberg, began developing a tool to overcome this problem. Initially targeting a glutamate receptor called mGluR2, they developed a tethered ligand—a receptor-activating molecule of glutamate attached to one end of a long, flexible stalk including a photoswitchable group called an azobenzene. This “glutamate-on-a-leash” arrangement could be chemically anchored to a labeling tag on mGluR2. When hit by light of different colors, the azobenzene would bend or straighten, bringing the glutamate into or out of the binding pocket of mGluR2, thereby switching the receptor on and off. To restrict this switching to cell types of interest, the tethered ligand was anchored to special labeling tags that can be genetically-encoded so that it would appear only on precisely defined cell types. The scientists called their tool a photoswitchable, orthogonal, remotely-tethered ligand—“PORTL.”
“We used the power and versatility of organic chemistry to precisely design and synthesize molecules with tunable and well-defined properties,” said Dr. Broichhagen.
In their new study, Drs. Levitz, Broichhagen and co-first authors, Amanda Acosta-Ruiz and Vanessa Gutzeit, Weill Cornell Graduate School of Medical Sciences doctoral students, greatly improved the efficiency of PORTL technology by making the anchor protein more flexible and increasing the number of their “glutamates-on-a-leash”—turning it into a two- or four-branched structure. They showed that with the new PORTL tool they could activate mGluR2 receptors with near-perfect efficiency, and activate mGluR3 and mGluR5 receptors as well.
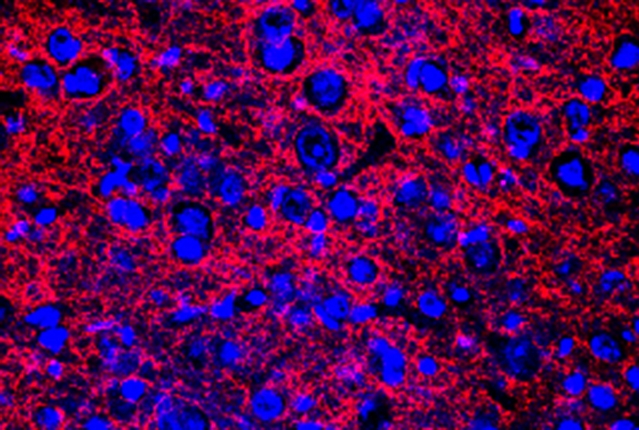
“With these novel structures that bear multiple photoswitchable units, we have overcome previous limitations of efficiency of our PORTL system. We anticipate this as a general approach to boost activation of receptors to the full level,” said Dr. Broichhagen.The scientists also showed that they could incorporate a fluorescent beacon on the PORTL structure, allowing them to track the specific locations of the receptors being activated, and, if desired, activate them only in tiny zones on cells. In this way they found that individual, mGluR5-bearing “arms” of astrocytes, star-shaped helper cells in the brain, can work as distinct subcellular signaling units.
“This is something we would never have discovered without a targetable activation method like PORTLs,” Dr. Levitz said.
The team demonstrated the new PORTL tool in mice, using it to activate mGluR2 receptors on precisely defined neurons in the medial prefrontal cortex. They showed with behavioral experiments that this specific sub-population of prefrontal neurons is likely the one that mediates the effects of mGluR2-targeting schizophrenia drugs currently under development.
“Essentially we now have a method for dissecting how GPCR-targeting antipsychotic, antidepressant or anti-anxiety drugs work,” Dr. Levitz said.
Apart from being a tool for studying drug mechanisms and basic neuroscience, the technique, Dr. Levitz noted, can be used for new drug development by identifying the specific brain cell populations that should be targeted by a drug and which other, “off-target” cells are likely to cause side effects.