Dr. Carl Nathan, chair of the department of microbiology and immunology and the R.A. Rees Pritchett Professor of Microbiology at Weill Cornell Medicine, has co-authored a review in Science on the immune protein interferon-gamma. He answered questions about its history and prospects as a therapeutic.
How was IFN-γ's basic biological role discovered?
In 1969-1971, while I was in medical school, I addressed a central mystery of the period: How do lymphocytes recognizing a specific infectious agent prepare macrophages, a type of phagocytic cell, to increase their capacity to kill bacteria and parasites without regard to whether the infectious agents were the ones that the lymphocytes recognized? I tracked this activity to a secreted protein I called macrophage-activating factor (MAF), but I did not know its identity. I had to put the matter aside while I finished medical training.
Meanwhile, in 1957, scientists had discovered that virally infected chicken epithelial cells released a protein that warned nearby epithelial cells to defend themselves against the virus. They called the protein “interferon”. Between 1965-1975, it emerged that lymphocytes too could release a protein with a weak antiviral effect on other cells, but it was not the same as epithelial cell interferon and was named ‘interferon-gamma” (IFN-γ).

Dr. Carl Nathan. Credit: John Abbott
When I joined Rockefeller University in 1977, I returned to the problem I had studied in medical school. By 1983, I discovered that MAF was IFN-γ. Emerging techniques to knock out genes, produce pure proteins and make monoclonal antibodies converged to demonstrate that mice deprived of the ability to make or respond to IFN-γ lost much of their ability to resist a variety of bacteria and protozoa that their macrophages would otherwise control.
Two findings clinched the relevance of IFN-γ to human infectious disease. In 1986, I reported that giving IFN-γ to patients with leprosy rapidly cleared the pathogen from their macrophages. In 1996, Jean-Laurent Casanova began to identify mutations that reduce people’s ability to produce IFN-γ or respond to it, resulting in heightened susceptibility to certain pathogens.
How does IFN-γ fight pathogens?
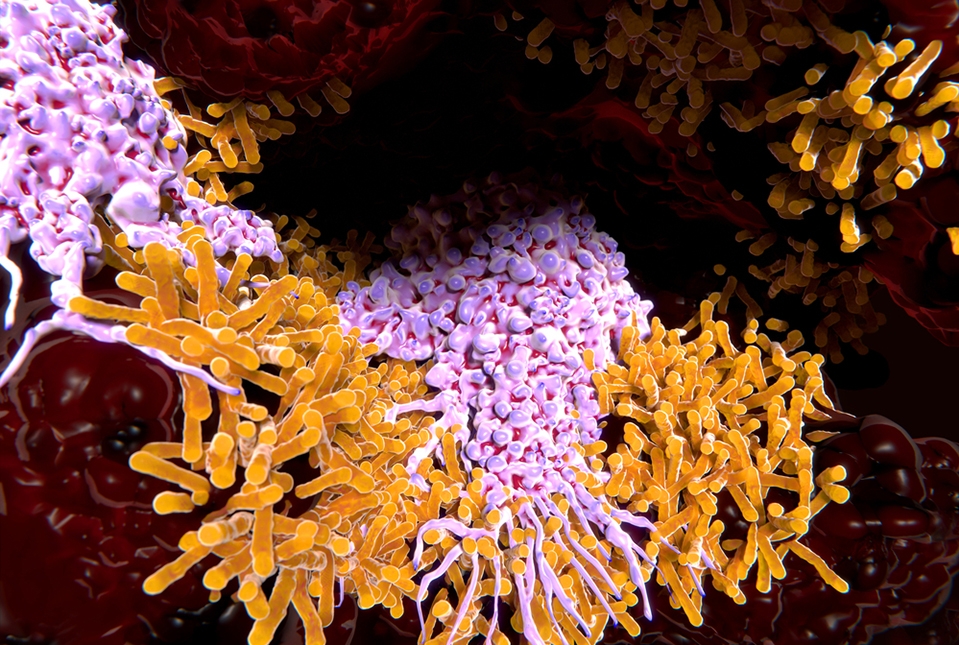
IFN-γ instructs cells to express hundreds of genes at higher levels. We only know what some of them contribute. It took me about ten years apiece to identify the two IFN-γ-induced mechanisms that are essential to survive infection: production of reactive oxygen species and reactive nitrogen species. My former student, Dr. John MacMicking, showed that a family of proteins called GBPs plays a critical role in amplifying these actions and those of a lipoprotein called ApoL1 in diverse kinds of cells.
What opportunities do you see for making better clinical use of IFN-γ?
When antibiotics were routinely effective, people did not pay much attention to the ability of IFN-γ to fight infection. IFN-γ was commonly used to treat rare genetic conditions, or rarely used to treat common infections encountered in countries with limited resources. Today, many infections are harder to treat because antibiotic resistance is spreading and many pharmaceutical companies have retreated from discovering new ones. Climate change drives diseases from their geographies and society has grown cognizant of global health. It’s time to consider wider use of IFN-γ.
At a personal level, this story is now 53 years old. That half century has given us a book with many authors, but it’s clear this will be a multi-volume series. Meanwhile, there are patients we can help.