A specific toxin-producing gut bacteria may be responsible for both triggering the onset of multiple sclerosis (MS) and ongoing disease activity according to a new study led by a team of researchers at Weill Cornell Medicine and NewYork-Presbyterian. The team is working with investigators from UC San Diego, UC Davis, the University of Pittsburgh, Cornell’s Ithaca campus and has a long-standing collaboration with scientists at The Rockefeller University.
The work, published Feb. 28 in The Journal of Clinical Investigation, identifies epsilon toxin-producing Clostridium perfringens in unusually high abundance within the gut microbiome of people with MS. The study goes on to show that in a preclinical model of MS, epsilon toxin opens the blood vessels of the brain allowing inflammatory cells to gain access to the central nervous system and cause demyelination characteristic of MS.
MS is a disabling disease of the central nervous system that commonly has its onset in young adulthood and affects nearly one million people in the United States alone. Early in the disease course, MS is characterized by episodic relapses and remissions of neurologic symptoms, including loss of vision, weakness, imbalance and others. Later in the disease course, despite numerous advancements in treatment, MS tends to progress in approximately 40 percent of afflicted individuals.
“There are many mysteries to MS,” said co-senior author Dr. Timothy Vartanian, a professor of neuroscience in the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine. “Why do some people get MS and others don’t, despite similar or identical genetics? What accounts for the episodic nature of relapses and remissions? How is the central nervous system targeted and why myelin specifically? Clostridium perfringens and epsilon toxin may explain many of these mysteries.”
An environmental trigger is required for MS to occur in a genetically susceptible individual, and the abundance of epsilon toxin-producing Clostridium perfringens in people with MS suggests it could be the culprit. Epsilon toxin-producing strains of Clostridium perfringens live in the small intestine, and epsilon toxin is only produced briefly when the bacterium is in a growth phase, fitting with the relapsing remitting nature of MS. Perhaps most remarkably, epsilon toxin specifically targets brain blood vessels and myelin, providing a clear mechanism of its action.
Despite the mounting evidence that epsilon toxin-producing strains of Clostridium perfringens could be relevant environmental pathogens for MS, modern studies of the gut microbiome in people with the disease failed to detect these strains. In the current study, Dr. Yinghua Ma, an assistant professor of research in neuroscience in the Vartanian lab, led work, along with co-lead authors Drs. David Sannino and Jennifer Linden in the Brain and Mind Research Institute, showing that more sensitive techniques readily detected these strains in the MS gut microbiome.
“Previous studies would use a method where you could see the bacterial species that are there, but you couldn’t actually see the toxin or some of the more functionally relevant parts of the species,” said co-senior author Dr. Christopher Mason, a professor of physiology and biophysics and co-director of the WorldQuant Initiative for Quantitative Prediction at Weill Cornell Medicine.
Using highly sensitive DNA detection techniques, Dr. Ma found that people with MS are more likely to carry epsilon toxin-producing C. perfringens in their small intestines than healthy controls.
“The team brought the full armamentarium of modern molecular biology to address the question of pathogenesis and possible drivers of multiple sclerosis,” said Dr. Mason, who is also a professor of neuroscience in the Brain and Mind Research Institute at Weill Cornell Medicine. Having established this correlation, the investigators tested whether the toxin alone could cause the disease.
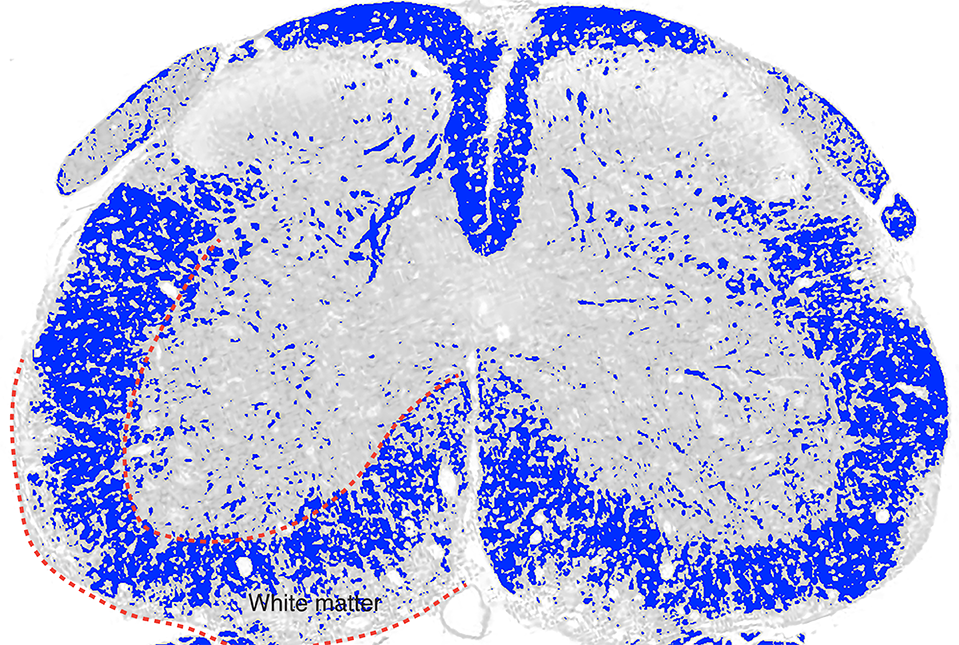
For that, they turned to a standard mouse model of MS in which animals are predisposed to autoimmunity, but MS-like disease only occurs if mice are also given pertussis toxin. Dr. Ma substituted epsilon toxin for pertussis toxin and animals developed a disease that more closely resembled MS compared to previous models.
“The finding that epsilon toxin can replace pertussis toxin in a mouse model of MS is very exciting,” said co-author Dr. Gregory F. Sonnenberg, the Henry R. Erle, M.D.-Roberts Family Associate Professor of Medicine and a member of the Jill Roberts Institute for Research in Inflammatory Bowel Disease at Weill Cornell Medicine. “It not only advances a more relevant model to study MS, but critically defines a new microbial-derived determinant that provokes a breakdown of immune privilege in the central nervous system to initiate demyelinating disease.”
“Epsilon toxin functions at the very earliest stage of MS lesion formation,” said Dr. Vartanian, who is also chief of the Multiple Sclerosis and Neuro-Immunology Division in the Department of Neurology at Weill Cornell Medicine and a neurologist at NewYork-Presbyterian/Weill Cornell Medical Center. “A treatment that neutralizes epsilon toxin may halt our patients’ new disease activity, far more effectively than current treatment modalities that suppress or modulate the immune system.”
“In the immediate term, we’re driven by a sense of urgency to get more effective and safer therapeutics to people with MS,” said Dr. Vartanian.
Dr. Tim Vartanian and Dr. Yinghua Ma are co-founders and equity stakeholders for Astoria Biologica. Dr. Vartanian and Dr. Ma are also inventors on a patent application for the method used to diagnose and treat multiple sclerosis.