A molecule promoting blood vessel growth in bone can create an environment suitable for bone-building formation, representing a potential target for new drugs to treat osteoporosis and fractures, according to new research by Weill Cornell Medicine scientists.
The findings, published May 21 in Nature Medicine, show that a substance, which is best known for spurring nerve growth, called SLIT3, both reversed the bone-weakening effects of osteoporosis and helped fractures heal when administered in mice. The multi-center research effort could fuel drug development efforts targeting the SLIT3 pathway in humans, enabling a new approach for blood vessel-directed therapy to treat bone loss, persistent fractures and fragile bones.
Existing drugs for osteoporosis work in one of two ways: Either they block the cells that destroy bone or they promote bone formation by cells called osteoblasts. “But only those promoting new bone formation will help you actually heal a bone fracture,” said co-senior study author Dr. Matthew Greenblatt, an assistant professor of pathology and laboratory medicine at Weill Cornell Medicine. “Our findings have potentially demonstrated a third category: drugs that target blood vessel formation within bone, prompting new bone to form.”
Osteoporosis, which causes bones to thin and become brittle, leads to nearly 9 million fractures worldwide each year, or one every three seconds, according to the International Osteoporosis Foundation. Women are disproportionately affected, and the risk increases with age. One in two women and one in five men will have an osteoporotic fracture during their lifetimes, and these fractures kill as many women each year as breast cancer.
“Osteoporosis and skeletal fractures due to osteoporosis are both common and deadly,” Dr. Greenblatt said.
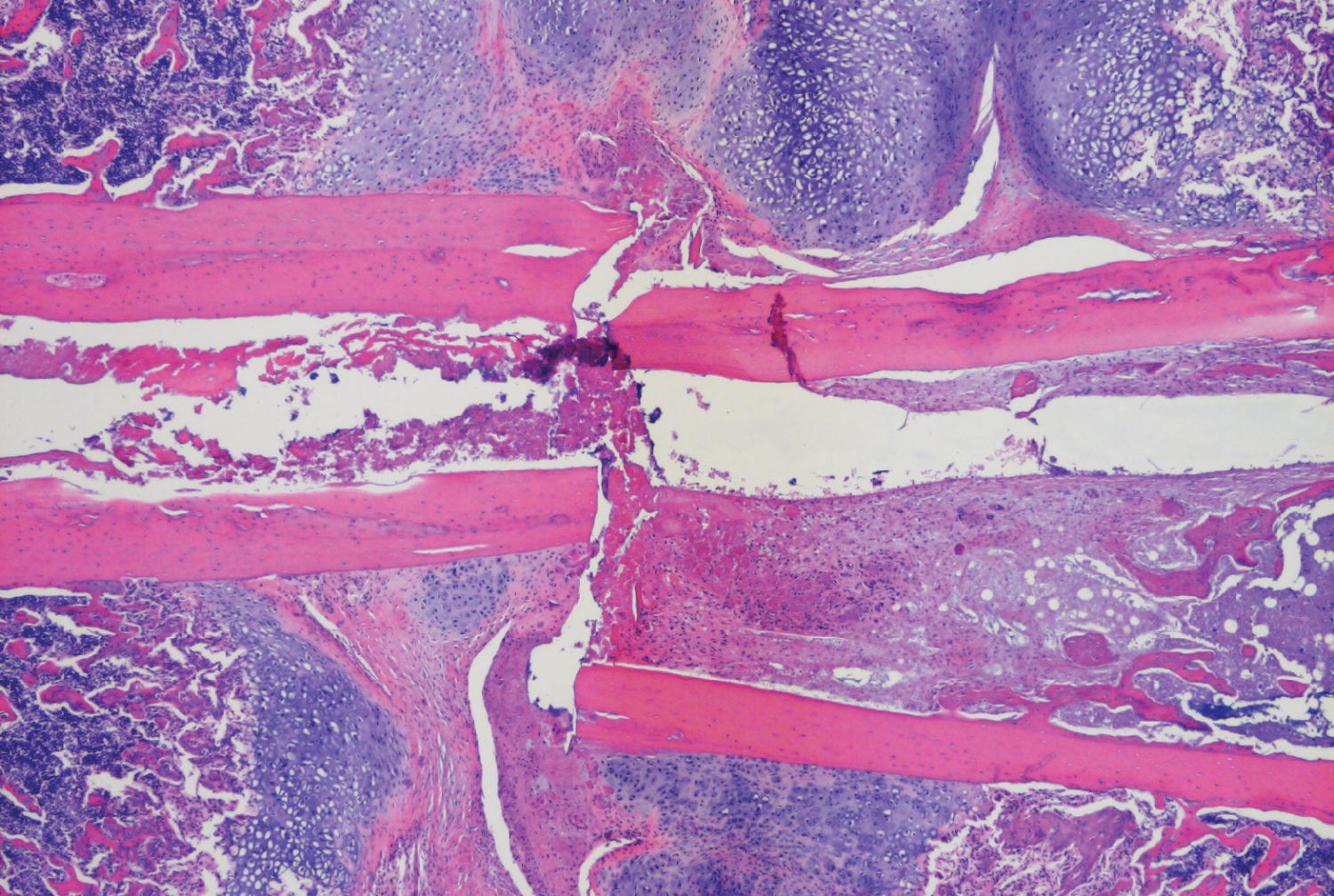
To counteract that trend, Dr. Greenblatt has been investigating the cellular causes of osteoporosis in an effort to promote bone growth. Prior research using mice genetically engineered to lack an adaptor protein known as SHN3 showed that its absence conferred high bone mass. Building on that discovery, Dr. Greenblatt and his team decided to examine the resulting changes in bone blood vessels. “We used those mice as a means to find the signals coming from osteoblasts to control the specific type of blood vessels present in bone,” he said.
The researchers were surprised to find that osteoblasts secreted unchanged amounts of almost all known factors promoting blood vessel growth, but SLIT3 levels rose significantly. And when the mice were genetically altered to delete SLIT3, they exhibited low bone mass. “We next asked if we could use SLIT3 to treat mice with skeletal disease, especially osteoporosis and fracture healing,” Dr. Greenblatt said. “When we gave the rodents SLIT3, it reversed their osteoporosis and made their fractures heal faster and stronger.”
“To my knowledge, this is the first example that we can develop a drug to treat bone disease in mice not by targeting the bone-forming cells,” he said, “but instead by targeting special types of blood vessels that exist in bone.”
Further research is needed to determine the best way to deliver SLIT3 to the bone in humans. SLIT3-pathway drugs could also be used in combination with existing drugs to improve patient outcomes.
“Only a small fraction of patients who’ve had a hip fracture and really require medication to prevent additional fractures get the drugs they need. Many people aren’t aware of how debilitating and deadly these kinds of fractures are,” Dr. Greenblatt said. “Having a totally new category of bone drugs that work on different sets of cells could open up new opportunities for treatment.”
In addition to benefiting seniors with osteoporosis, Dr. Greenblatt hopes his research will also help patients with bone injuries that aren’t healing properly, such as those who’ve undergone orthopedic surgery or have fragile bones due to genetic diseases. “Some of those people’s fractures don’t heal because they can’t grow the right type of blood vessels at the site of the fracture,” he said. “That’s what we think SLIT3 will do: help with that growth and promote healing.”