By Anne Machalinski
Photos By John Abbott
On a Tuesday in early June, just days before summer break, dozens of third-year medical students gathered in the Belfer Research Building to present findings from independent research projects they’d been working on since February. One student compared the use of palliative care in oncology in the United States and India; another presented findings on a promising biomarker that might allow physicians to track the progression of a pediatric brain tumor; and a third described her investigations into whether large polyps are a risk factor for metastatic colorectal cancer.
The poster session was the culmination of the first part of a six-month, dedicated research block that all Weill Cornell Medical College students now participate in during their third year. Begun in 2014, this capstone requirement is called the Areas of Concentration (AOC) program. It requires students — with the exception of MD-PhDs — to pick an area in which they’d like to gain in-depth knowledge, then complete original research related to it before graduation under the tutelage of a one-on-one mentor. “The more we can educate students in how to conduct original research,” says Dr. Anthony Brown, an associate professor of cell and developmental biology and the director of medical student research, “the more likely our graduates will be to challenge the status quo, make advances in their fields and become better doctors.”
The AOC is the latest in a continuum of changes to the curriculum at Weill Cornell Medical College — which, like many of its peer institutions, has shifted away from a classroom-focused system for the early years of medical school. Today, medical educators generally accept that students should be exposed to clinical work as early as possible. Protected research time, a relatively new concept in medical education, is also considered a benefit for physicians-in-training. Although many schools only require a few weeks or months, often broken up by other coursework, Weill Cornell Medical College — which previously didn’t require any research at all — opted to add six months. Students now do four months of research in the spring of their third year and two in the fall of their fourth, then report their work in a scholarly paper. “As a med student, I’ve sometimes felt like I’m memorizing all this information and just trying to retain as much as I can,” says Marta Dzyadyk ’18, who presented research on beneficial microbes that live in the gastrointestinal tract. “But the AOC program allowed me to ask a research question and think a little more creatively. I loved being in a basic science lab and taking ownership of my project.”
Professor of Medicine Dr. Andrew Schafer, who is the program’s director, stresses that in no way is the AOC intended to pressure students to choose a specialty prematurely, or push them into full-time research. Instead, he says, it gives medical students a chance to do what PhD candidates have been doing all along: thinking about the big picture, and creating — rather than just absorbing — knowledge. “A lot of medicine today ends up being very technical,” he says, “but we want all of our graduates, including doctors going into clinical practice, to maintain a scholarly and scientific perspective in their careers.” This means continuing to ask fundamental questions that might advance clinical standards; working with scientists to translate promising research into improved treatments for patients; and maintaining strong ties with a scholarly scientific community, like the one that the AOC program invites students to join. “Medical school is the perfect time to ingrain this out-of-the-box way of thinking,” Dr. Schafer says, adding that the AOC also builds confidence, grounds students in the fundamentals of the research process and strengthens their CVs, giving them a boost when they apply for fellowships and residencies.
An Evolving Educational Landscape
Introduced in the first weeks of medical school, the AOC program starts by linking students with one of four “exploratory advisers”: Dr. Brown (who works with students wanting to focus on laboratory research); Dr. Mark Pecker, clinical professor of medicine (clinical research); Dr. Madelon Finkel, professor of clinical healthcare policy and research (global and public health, health policy, and population research); and Dr. Schafer, who takes students who are undecided. As students work through their foundational science classes, they periodically meet with their adviser to pinpoint their choice from a list of about 50 areas of concentration including nanomedicine, communication disorders, geriatrics and addiction medicine. Their adviser also helps them find a faculty mentor, who will work with them on the scholarly project they propose in the fall of their third year. Dr. Brown notes that after having completed 12 months of clinical clerkships, most students are ready to slow down and think creatively — a reprieve that the research block, which begins in February, provides. “Students look at this as a breath of fresh air in what is an otherwise very stressful curriculum,” he says. “They take advantage of what is essentially a giant block of unstructured time, and enjoy the process of creating knowledge.”

Vince Raikhel ’18 (center) with mentors Dr. Susan Ball (left), and Dr. Milagros Silva
For Sydney Ariagno ’18, a Dallas native who came straight to medical school from her undergraduate studies at Washington University in St. Louis, the AOC program was a major reason she chose to attend Weill Cornell Medical College. She conducted neuropsychology research in college, studying biomarkers that turn up in the blood of pediatric patients after a concussion to see how they correlate with cognitive function later on. At Weill Cornell Medical College, she decided to try basic science research, to learn new skills and see if she enjoyed the process. Dr. Schafer guided her toward cancer research; then Dr. Brown introduced her to her eventual mentor, Dr. David Lyden, the Stavros S. Niarchos Professor in Pediatric Cardiology at Weill Cornell Medicine and a pediatric neuro-oncologist at Memorial Sloan Kettering Cancer Center. After learning about his work on exosomes — microparticles released by tumor cells — she knew she’d found the right fit. “Dr. Lyden’s research interests are very much in line with what I was hoping to focus on,” says Ariagno, who plans on going into pediatrics or pediatric oncology after graduation. “Our meeting went so well that I didn’t need to consider working with anyone else.”
The project Ariagno focused on during her research block — which she has extended into a full year, after which she’ll return to her medical studies — is on medulloblastoma, the most common malignant pediatric brain tumor. Along with Dr. Lyden and co-mentor Dr. Praveen Raju, an assistant professor of pediatrics at Weill Cornell Medicine, Ariagno is looking at whether exosomes released by this tumor could be detected by a blood test — not only to diagnose it, but to monitor whether it has grown or spread after treatment. “This is a really collaborative project; I get to work with both of my mentors equally,” says Ariagno. “Dr. Lyden’s lab is focused on general cancer biology and the mechanisms of cancer progression, and Dr. Raju focuses on medulloblastoma and brain tumors. It’s been illuminating to see both the broad and more narrow questions play out in the research, and consider how this lab-based work could lead to a safer, non-invasive way of diagnosing and monitoring kids with this type of tumor.”

Dr. Andrew Schafer (left), with students Caitlin Gribbin ’18 (center) and Aditi Gupta ’18
While AOC leaders say it’s too early for a comprehensive assessment of the program’s benefits, it seems to be paying off. This year, five third-year students, including Ariagno, received Howard Hughes Medical Institute fellowships, each providing $32,000 to support a year of research. Two more third-years received other prestigious fellowships, one from the Sarnoff Cardiovascular Research Foundation and another from the Doris Duke Charitable Foundation. In the past, only one or two students per year were likely to receive such honors, Dr. Schafer says. “We can’t take full credit for this increase — but we did get students to start thinking about research early, made them aware of these opportunities, helped them with their applications and urged them to apply,” he says. “This is an early indicator of success that shows we’re on to something.”
Shooting for the Stars
While many incoming students are unsure about their future specialty, Tim Donahoe ’19 stands out for his singular focus: he wants to be an astronaut. Even before he matriculated, he outlined what he hoped to do in aerospace medicine and reached out to Weill Cornell Medicine’s three astronaut alumni. He also identified a faculty mentor: Dr. Christopher Mason, an associate professor of physiology and biophysics who is one of the lead investigators of the NASA Twins Study, which studies how long-term space flight affects the human body (in astronaut brothers Scott and Mark Kelly) and is developing new technology for DNA diagnostics in space. After Dr. Mason eagerly took him under his wing and they brainstormed a research outline, Donahoe set up a meeting with Dr. Schafer to describe his plan. “He was a little surprised, because no student had visited him yet — and I came in with this whole plan that I was super excited about,” says Donahoe. “But he was also extremely supportive, and within a month the school launched an aerospace medicine and space genetics area of concentration.” The summer before his third year, Donahoe spent a week shadowing an astronaut who’s also a physician at the Johnson Space Center — an experience facilitated by Dr. Ellen Baker, (MD ’78), a veteran of three space missions. Now, he’s deciding whether to spend his upcoming research block studying genomic changes in astronauts during space flight or comparing zero-gravity exercise regimens — knowledge that’s meant to elucidate what would happen to the human body on a long-duration mission to Mars, for example.
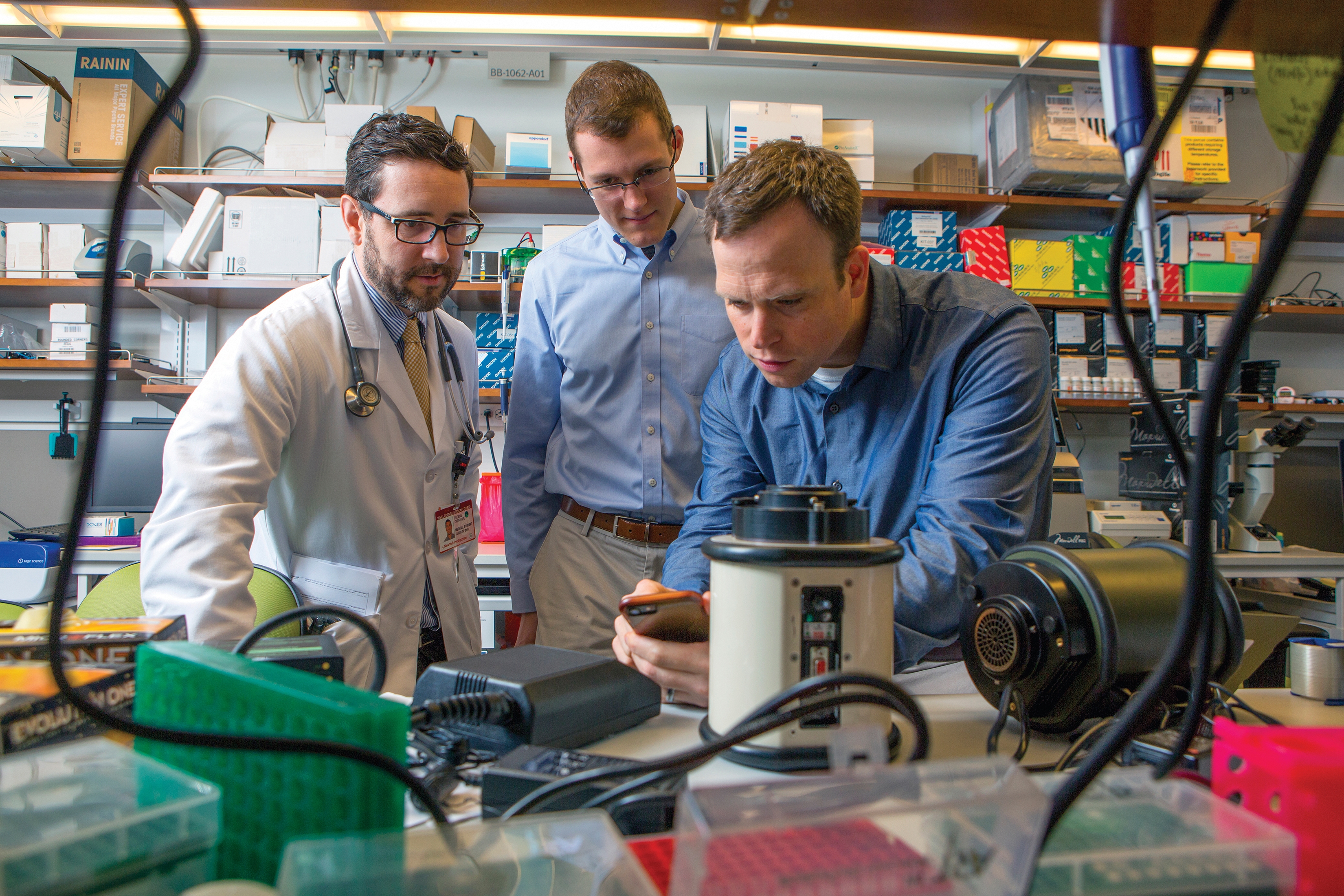
Eugene Carragee ’18 (left) and Tom Donahoe ’19 with mentor Dr. Chris Mason (right)
While such research may seem distant from the practice of medicine on Earth, it provides practical insights for future doctors, says Eugene Carragee ’18, an aspiring anesthesiologist who also is pursuing an aerospace AOC. “Learning what happens when someone goes into space, and the compensatory mechanisms that kick in because of a micro-gravity environment, has helped me understand much better how the body works and how the organ systems interact with one another,” says Carragee , who is working with Dr. Mason on the Twins Study. “I see this in-depth knowledge as a bridge between what I’ve done in this concentration and what I’ll pursue as a specialty.”
Joining a Research Community
When AOC leadership unveiled the program in 2014 after a long planning process, Dr. Schafer feared it would be challenging to find faculty willing to participate. But he had the opposite problem: there was a rush of volunteers. Among them was Dr. Harjot Kaur Singh, an assistant professor of clinical medicine who leads the infectious diseases AOC with Dr. Laura Kirkman, the William Randolph Hearst Foundation Clinical Scholar in Microbiology and Infectious Diseases. The pair welcomed six students by inviting them to participate in division meetings and to share their work at a gathering two days after the poster session. “We thought this was a great opportunity — not only for students to showcase what they’ve done, but also for the infectious diseases group to offer mentorship, support and advice,” Dr. Singh says.
For Dzyadyk, the third-year student who studied gut microbes as part of the infectious diseases AOC, the program’s biggest benefit has been developing close relationships with her mentors at Memorial Sloan Kettering Cancer Center: Dr. Eric Pamer, an infectious diseases physician, and Dr. Miriam Torchinsky, a fellow. Both not only guided her through her research, but shared details about their professional paths and advised her on topics like identifying her own interests and choosing a specialty. Says Dzyadyk: “Graduating from medical school, we’ll earn an MD — but there’s still so much more to learn about medicine, ourselves and what we want to do in our careers.” Vince Raikhel ’18 had a similarly powerful mentorship experience — halfway around the world. After spending two months shadowing a palliative care physician in New York, he spent six weeks doing the same in Vellore, India. From both, he learned the importance of slowing down to get to know the patient and involving families in the medical decision-making process, an experience he calls “very inspiring.”
In addition to faculty mentorship, a key part of the AOC is that students help and support each other. At biweekly meetings during the research block, groups of seven to 10 students brainstorm solutions to research problems, with a faculty facilitator on hand to offer advice. Natalie Wong ’18 needed that peer input — as well as guidance from her mentor, Dr. Heather Yeo, an assistant professor of surgery and the Nanette Laitman Clinical Scholar in Healthcare Policy and Research/Clinical Evaluation — when she realized that her proposed project wasn’t going to work out. Wong originally set out to study complications related to colorectal cancer screening procedures using a massive national database, but realized that the dataset was missing a lot of variables that she needed to do the correct analysis. So, working with her mentor, she shifted to another question, for which the data was more helpful: are large polyps a risk factor for metastatic colorectal cancer that has spread to the lymph nodes? Physicians working with Dr. Yeo’s group are keenly interested in the answer, which could impact clinical practice. Says Wong, who’s continuing her research this fall: “Hitting roadblocks and working through them has been an important part of my experience.”
This story first appeared in Weill Cornell Medicine, Vol. 16. No. 3

