By Elaine Meyer
Photos by John Abbott
Soon after the first case of COVID-19 was reported in New York City last March, a group of about 10 physician-scientists at Weill Cornell Medicine met to discuss a pressing issue: there were no known treatments for severe cases of the disease. At the time, such cases had a dangerously high chance—around 25 to 40%—of leading to death or to lasting complications like severe lung damage. At the meeting, the enormity and the urgency of the situation came into stark focus. The infectious disease specialists anticipated that Weill Cornell Medicine, and New York City, could face the same situation as had overwhelmed hospitals in northern Italy—though they didn’t expect that it would happen as quickly as it did. To prevent death on a scale previously unimaginable in their medical careers, they began to discuss how they could acquire and study—as soon as possible—treatments for a virus the world was just beginning to understand.
Normally, clinical research on therapeutics takes years. But SARS-CoV-2, the virus that causes COVID-19, wouldn’t allow for this kind of timeline. As the number of patients hospitalized with the virus at NewYork-Presbyterian/Weill Cornell Medical Center shot up in early March 2020, Weill Cornell Medicine became a research hub for the rigorous investigation of COVID treatments and, later, two top vaccine candidates.
Results from those studies have contributed to a growing body of knowledge from around the world that has improved the care doctors can provide—in some cases enabling them to prevent or reduce the severity of disease and even the percentage of patients who die of COVID. Additionally, strong early results reported from the Moderna vaccine trial, in which Weill Cornell Medicine participated, along with the trial of a vaccine by BioNTech and Pfizer, may pave the way to the eventual end of this global health crisis. “To do clinical trials in the middle of a pandemic was just extraordinary,” says Dr. Roy Gulick chief of the Division of Infectious Diseases and the Rochelle Belfer Professor in Medicine at Weill Cornell Medicine and an attending physician at NewYork-Presbyterian/Weill Cornell. “You had a swell of very ill people with a highly contagious disease whose infectivity and typical clinical course we didn’t yet know. At the same time, while critically ill people often will want to try anything, including investigational drugs, to get better, they usually want to talk over participation in a clinical trial with their families and friends—and providers want to have comprehensive discussions with their patients about participating. So this was a really challenging environment.”
In Record Time
Soon after the infectious disease faculty met, 12 experts in areas ranging from rheumatology to pulmonology reviewed more than 70 ideas for potential treatments from across the medical center. The group—dubbed the COVID-19 Clinical Trials Task Force—prioritized studies that were scientifically sound and compelling, either government-sponsored or initiated by Weill Cornell Medicine investigators, and not too duplicative of studies elsewhere. “There’s a reason that we conduct rigorous scientific research, and it’s because you don’t know at first blush how effective an agent will be,” says Dr. Rainu Kaushal, senior associate dean of clinical research, who is also the Nanette Laitman Distinguished Professor of Population Health Sciences and chair of the department. “At Weill Cornell, we believe in the process of science; we’re leaders in the process of science, and COVID is an example of that. The work we have done demonstrates the strength of our expertise in clinical care delivery, clinical trial development, and deployment in population and health services research.”
The task force was especially hopeful early on about two drugs, remdesivir and hydroxychloroquine, which had performed well in laboratory studies by blocking steps in the life cycle of SARS-CoV-2. Remdesivir had also showed activity against the coronaviruses that cause Severe Acute Respiratory Syndrome (SARS) and the Middle Eastern Respiratory Disease (MERS) and had proven safe, though not effective, in clinical trials of Ebola patients. Hydroxychloroquine was already approved by the Food and Drug Administration to treat lupus and rheumatoid arthritis and so was readily available.
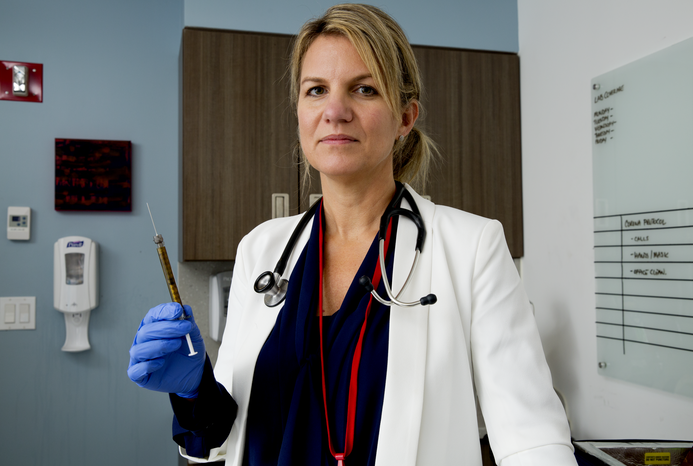
But given that SARS-CoV-2 was a new virus, there was no evidence as to whether either drug would be effective in humans; this would require studying it in patients, and not just a lab. “One lesson COVID has reinforced is that a lot of things work in test tubes. But that doesn’t necessarily mean they’re going to cure someone or be effective in treatment,” says Dr. Kristen Marks, (MD, MS ’09), an associate professor of medicine in the Division of Infectious Diseases at Weill Cornell Medicine and assistant attending physician at NewYork- Presbyterian/Weill Cornell, who led studies of remdesivir and is now leading the medical center’s vaccine trials.
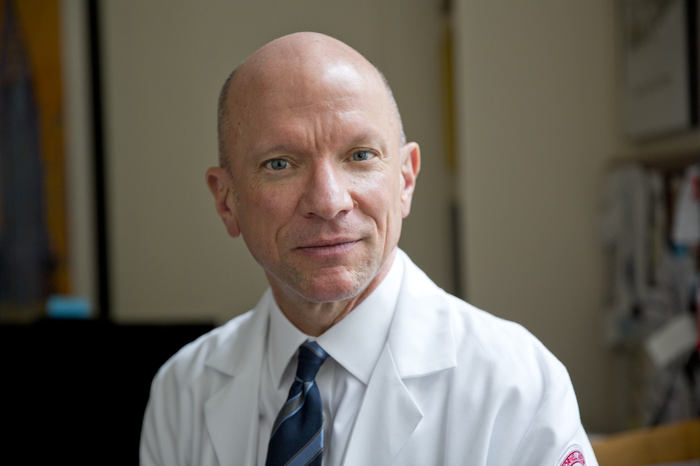
Dr. Roy Gulick. Credit: John Abbott
To get these studies up and running at “hyper speed,” faculty and staff made enormous pushes, says Dr. Gulick. Research teams that ran clinical trials on HIV, transplant oncology, and other infectious diseases were shifted to the COVID trials. Some were housed in hotels near the medical center so they could be close to work while they drafted research protocols that would be evaluated by Weill Cornell Medicine’s Institutional Review Board (IRB), and because at the time there were concerns they might expose their families to the virus. “That showed enormous dedication, staying in hotels for weeks at a time, working seven days a week; it was an incredible team effort,” says Dr. Marshall Glesby, a professor of medicine and of population health sciences at Weill Cornell Medicine and an attending physician at NewYork-Presbyterian/Weill Cornell who ran trials of some of the experimental treatments. Weill Cornell Medicine’s IRB and contracts office also worked at rapid speed, approving the protocols and contracts for the studies less than a week after submission.
As the researchers note, enrolling patients was more challenging than in a typical clinical trial. Early on, remdesivir supplies were limited because the drug wasn’t yet FDA approved, restricting how many patients could enroll. As part of informed consent requirements, research staff also had to explain to potential participants that they did not know whether the therapies would work—a particularly harrowing reality given the rapid deterioration of some COVID patients—but that was a risk that many were willing to take, Dr. Marks says.
The process was complicated even more because, to limit exposure, patients’ families couldn’t be in the same room to discuss options with doctors. In some cases, patients were close to being put on a ventilator or were already sedated, requiring a relative to authorize the patient’s participation in the study. Though in-person consent is normally required, families were able to give “e-consent” over videoconference, phone, or chat technology. “I spent a lot of time having people call their loved ones, to help them reach who they needed to, so they could feel good about the decisions they were making,” Dr. Marks says. “Often it was a very time-pressed situation. I had people from whom I would go in to get consent, and they would liter- ally be intubated an hour later, sometimes minutes later. I was incredibly moved by the bravery of the people who were willing to participate in research at a critical time.”
The study of remdesivir, published in the New England Journal of Medicine in early November by Dr. Marks and co-authors from around the world, reported that about 400 patients showed clinical improvement on either five or 10 days of treatment. The FDA used this and other studies to approve remdesivir in October as the first drug to treat COVID. The World Health Organization recently cast doubt on remdesivir’s effectiveness given its lack of mortality benefit and its cost, but the FDA and other scientists believe, based on the data, that the drug can speed recovery from the illness—an important clinical goal.
Other experimental treatments proved less successful. Weill Cornell Medicine investigators stopped their trial of hydroxychloroquine after evidence emerged from other hospitals that it wasn’t working. Investigators found in another study that sarilumab, an immunomodulator that had initially seemed promising, wasn’t effective for patients with severe illness—the population in which it was tested—and the treatment was stopped. Of course, the fact that some treatments may prove ineffective is a risk of participating in clinical trials. During an unprecedented pandemic like COVID, when so many unknown treatments are being tested at the same time, researchers have used what is called an “adaptive” trial design so patients can be switched to more effective options if they become available during a study. When it’s clear a therapy is ineffective, patients are immediately switched off, as was the case in the sarilumab study. “It’s important to know that a particular drug is not going to be a viable approach,” says Glesby, who ran the sarilumab trial and recently led a trial of convalescent plasma that was stopped early after the research showed it was unlikely to benefit patients. “Not only to physicians, but to patients and their families.”
Quest For a Vaccine
NewYork-Presbyterian/Weill Cornell is the only medical center in New York City participating in the trial of the Moderna vaccine, which enrolled over 30,000 participants across the United States and whose early results were much stronger than anticipated. In November, Moderna, which developed the vaccine in partnership with the National Institutes of Health (NIH), announced it is 94.1% effective in preventing COVID-19 illness, and the FDA authorized its emergency use in December. Among those who received two injections, only 11 participants were infected with COVID, compared to 185 in the group that received the matching placebo, according to data published in the New England Journal of Medicine in December. This is significantly more effective than the 30% to 60% risk reduction of a typical flu vaccine. Though new SARS-CoV-2 variants have emerged that could eventually challenge the efficacy of vaccines, many public health experts believe the distribution of the Moderna vaccine, and a similarly successful vaccine by Pfizer and BioNTech, will allow societies to control and possibly end the pandemic.
These enormous stakes are what drove Rose Strickland, an 81-year-old retired nurse, to volunteer to participate in the Moderna study. “We are in the midst of the worst pandemic of my lifetime. The only way we will be able to find some answers and possibly a treatment is by trying to determine measures to address the problem,” the Brooklyn resident says. “I feel we owe it to our frontline healthcare workers and scientists to do everything within our power to assist them in their efforts to maintain our health and wellbeing.”
Until now, the mumps vaccine held the speed record for development and approval: four years. Normally, it takes months just to test a vaccine’s biological mechanism and safety—two stages required before testing it on patients to see if it prevents infection and illness. Once participants are enrolled, they are randomly assigned to a group that receives the vaccine or to one that receives either a placebo or the current standard treatment. Even after efficacy data becomes available, investigators continue to monitor participants to determine how long the vaccine’s protection might last and whether they experience side effects.
For the Moderna study, Weill Cornell Medicine was determined to enroll a diverse population, given that the virus has disproportionately impacted the elderly, Blacks, and Latinos. This includes Strickland, who is Black and has hypertension. “I felt very strongly about contributing to ensure that participants are representative of the population,” she says. “My position is, I must participate because if I and others like me do not, we will have no assurance that when a vaccine is developed it will be as safe and effective for us as it is for anyone else.”
Weill Cornell Medicine investigators were interested in joining Moderna’s trial because its vaccine (along with Pfizer and BioNTech’s) uses synthetic messenger RNA (mRNA), a fairly new strategy that has never before been employed in an approved vaccine. The vaccine consists of a piece of the genetic template of the virus (in the form of mRNA) that is injected and then read by human cells to make the spike protein of the SARS-CoV-2 virus. Since only the viral spike protein is made, the vaccine itself can’t cause COVID-19. The viral spike protein stimulates the human immune system to generate a response in the form of specific antibodies and cells, which then are capable of identifying and destroying the actual virus if someone is subsequently exposed to it. Because mRNA technology is relatively quick and inexpensive—and may be safer than traditional vaccines that use weak or dead virus material—its FDA approval for Emergency Use Authorization in December represented a scientific milestone.

Vital Contribution: Retired nurse Rose Strickland (left) has a blood sample taken as part of the Moderna vaccine study, for which she volunteered.
Weill Cornell Medicine is also the site for a trial of a vaccine developed by Novavax that uses proteins from the SARS-CoV-2 virus; the trial started in late December and enrolled 30,000 participants at 115 sites across the continental United States, Puerto Rico and Mexico. According to several of the investigators involved, the NIH—which is coordinating many of the vaccine trials—chose Weill Cornell Medicine because of the medical center’s strong record for enrolling and managing clinical research as part of the AIDS Clinical Trials Group and the HIV Prevention Trials Network; both are initiatives of the National Institute of Allergy and Infectious Diseases (NIAID) and are working with other NIAID-funded clinical trials networks to test COVID-19 vaccines and treatments.
Although there have been concerns about the speed of vaccine approval, Weill Cornell Medicine faculty are adhering to rigorous standards of clinical research, just on an accelerated timeline. “No safety steps are being skipped,” says Dr. Marks, who is leading both of Weill Cornell Medicine’s vaccine trials. “What has changed to accelerate vaccine availability is that the phases of studies were overlapped and production of the vaccine began immediately.” No one is deliberately exposed to the virus—that would entail a different type of study, known as a “challenge trial”—and participants are told to continue practicing social distancing and wearing masks.
As Dr. Gulick notes, one of the realities of research in the time of COVID is that new results and developments happen at break- neck speed. “In clinical trials in the midst of a pandemic, literally anything can happen,” he says. “You have to be on your toes.” Investigators are nonetheless starting to consider how they can take some of the adaptations they made in the pandemic’s frenetic early days and establish new approaches that will make clinical research more responsive not just to COVID but to future pandemics. For example, the use of electronic consent processes—which helped speed up trial enrollment—may become more routine. The same goes for the use of adaptive study designs, in which investigators can switch patients from one experimental therapeutic to another (should a more promising option emerge) while still collecting clinically important data. Observes Dr. Timothy Wilkin, assistant dean for clinical research compliance and a professor of medicine at Weill Cornell Medicine and an attending physician at NewYork-Presbyterian/Weill Cornell: “We need to evolve from a ‘wartime’ operation to having a long-term plan and establishing some normalcy for how we do research.”
The scale, speed and severity of COVID, and the need to develop more treatments and vaccines, will continue to be an enormous test, even for clinical research infrastructures that have brought the rigor of modern science to controlling so many complicated and once deadly diseases. But, Dr. Kaushal says, at the end of a year of scientific discovery that was at times discouraging and at times politicized, this unprecedented clinical research effort is bearing fruit. “In response to a novel virus during a global pandemic, Weill Cornell Medicine brought together the scientific expertise of many specialties to test experimental therapies and translate the benefit to patients as swiftly as possible, sometimes in life-or-death cases. This is the kind of effort that is only possible at a collaborative and scientifically rigorous academic medical center.”
Sidebar: The Outlook for COVID Care - Treatments Target Disease on a Variety of Fronts
There are now a small but growing number of treatments for COVID-19 in hospitalized patients, including remdesivir in the virus’s earlier phase and dexamethasone and other corticosteroids in its later phase. But with the virus still raging in early 2021 and continued COVID-related deaths in the United States and many other countries, there is a need for strategies that can keep patients from getting sick enough to be hospitalized and reduce overall infection rates. Dr. Teresa Evering, (MD ’97), is running Weill Cornell Medicine’s arm of the ACTIV-2 study, a multicenter trial conducted by the AIDS Clinical Trials Group and sponsored by the NIH. ACTIV-2, which will investigate multiple agents, began with the study of Eli Lilly’s monoclonal antibody treatment, bamlanivimab. This investigational therapy involves cloning the most potent antibodies of people who have recovered from COVID in a laboratory, then infusing them into an infected person to block the virus from entering a cell and making copies of itself. “The goal of ACTIV-2 is to identify safe outpatient therapeutics that decrease the severity of COVID-19 and also decrease the duration of infection and the ability to transmit,” says Dr. Evering, an assistant professor of medicine at Weill Cornell Medicine and assistant attending physician at NewYork-Presbyterian/Weill Cornell. “We’d also like to see that they keep people from being hospitalized—and from dying.”
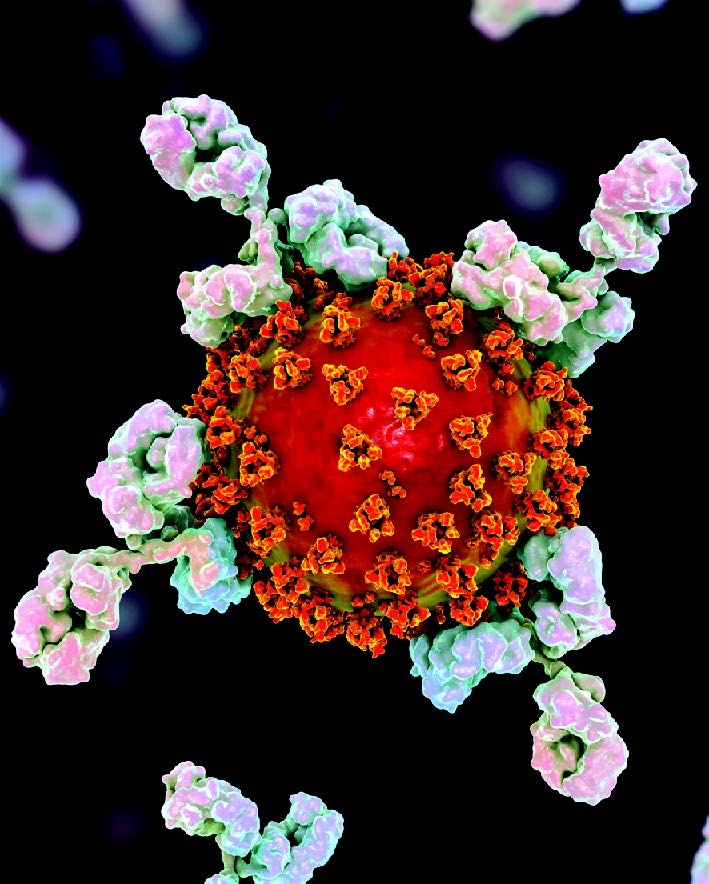
Defense Force: A conceptual illustration depicts antibodies attacking the SARS-CoV-2 virus.
Other strategies target the disease in the later phases characteristic of the most severe COVID cases. These patients typically develop an overreactive immune response to the virus, called a cytokine storm. Among many other complications, the reaction is linked to abnormal blood clotting—which can lead to strokes and to clots in the veins of the legs, arms, and lungs as well as the small pulmonary vessels, and can be fatal. Dr. Maria De Sancho, (MD, MS ’09), a professor of clinical medicine at Weill Cornell Medicine and a hematologist at NewYork-Presbyterian/Weill Cornell, is leading a clinical trial to determine what dose of anticoagulants (blood thinners) can be used to prevent excessive clotting and death in these patients without increasing the risk of bleeding. She is also studying patient blood samples to understand the mechanisms of clotting in people hospitalized with COVID.
Other Weill Cornell Medicine researchers are investigating the long-term effects of COVID, which range from neurological complications to organ damage, and are some of the most troubling and mysterious aspects of the disease. Dr. Alexander Merkler, (MD, MS ’20), an assistant professor of neuroscience and of neurology at WCM and an assistant attending neurologist at NewYork-Presbyterian/ Weill Cornell, and Dr. Babak Navi, (MD, MS ’15), an associate professor of neuroscience and of neurology at Weill Cornell Medicine, are leading a multi-site study to identify common risk factors for stroke in patients hospitalized for COVID. They hope to use the results to develop methods including a machine-learning algorithm that can help healthcare staff identify patients at high risk for stroke. Because half of patients who have had COVID show some kind of kidney damage, Dr. Robert Peck, associate professor of medicine and of pediatrics, is leading a study at Weill Bugando Medical College in Tanzania to identify the precise location of injury in the kidney and investigate whether it becomes a long-term health issue.
And Weill Cornell Medicine researchers are trying to understand how long patients are immune to SARS-CoV-2 after having COVID. While antibody tests can confirm whether someone was infected with the virus, it’s not clear how strongly these antibodies confer immunity. Dr. Julie Magarian Blander, the Gladys and Roland Harriman Professor of Immunology in Medicine, is studying blood collected from WCM and NewYork-Presbyterian/Weill Cornell healthcare workers who recovered from COVID. She is trying to understand if people with a receptor on certain immune cells that find and destroy cells infected with SARS-CoV-2 are immune to future infection. If successful, scientists hope to develop a more precise alternative to an antibody test that identifies people who are immune based on the presence of these receptors.