The activity of a gene called CIART is a key factor in the establishment of the viral infection that causes COVID-19, according to a study from researchers at Weill Cornell Medicine and New York University Grossman School of Medicine.
In the study, which appears March 13 in Nature Cell Biology, the researchers used multiple models of human organs, called organoids, to search for general host factors that influence infections by SARS-CoV-2, the coronavirus that causes COVID-19. They identified CIART as a strong SARS-CoV-2-enabling factor in organoids modeling both lung and heart tissue. The researchers traced CIART’s permissive effect on SARS-CoV-2 infection to its stimulation of the synthesis of small molecules called fatty acids.
“This finding demonstrates the power of a multi-organoid approach, by revealing a pathway that could be targeted with future drugs to treat or prevent SARS-CoV-2 infection across multiple organ systems,” said study co-senior author Dr. Shuibing Chen, the Kilts Family Professor of Surgery at Weill Cornell Medicine.
The other co-seniors of the study are Dr. Todd Evans, associate dean for research and the Peter I. Pressman, M.D. Professor in Surgery, and Dr. Robert Schwartz, associate professor of medicine in the Division of Gastroenterology and Hepatology at Weill Cornell Medicine; and Dr. Benjamin tenOever, director of the NYU Langone Virology Institute and a professor in the departments of microbiology and medicine at NYU Grossman School of Medicine.
SARS-CoV-2, like other respiratory viruses, typically initiates infection in the throat and sinuses. But it often spreads from the respiratory tract to other parts of the body, such as the gut, liver, heart, kidneys, brain, blood vessels and pancreas. Infections in these tissues are frequently seen in severe COVID-19 and can cause fatal complications including blood clots and organ failure.
“Different organs tend to respond differently to SARS-CoV-2 infection,” Dr. Evans said. “So, our idea was to look for factors that are relevant not just in one but in multiple organs.”
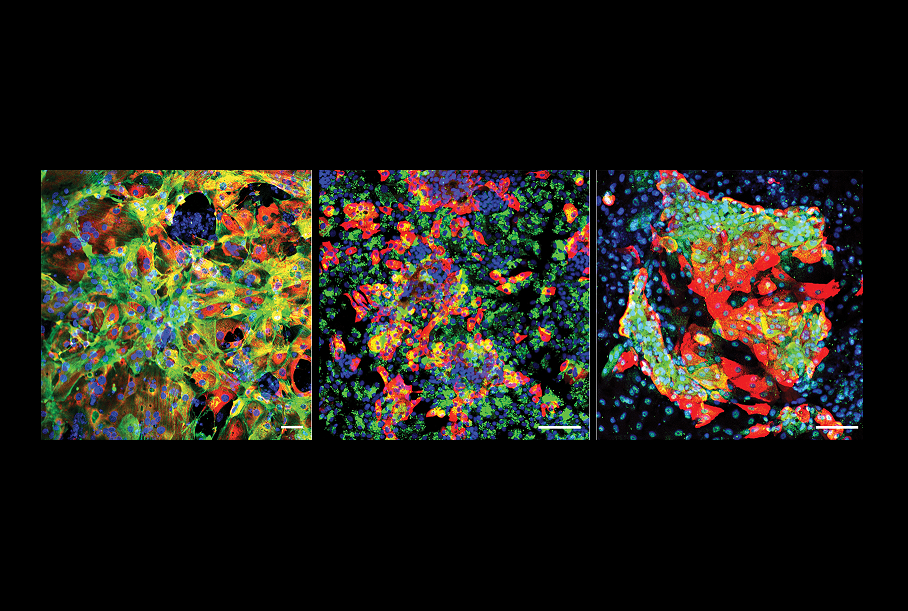
Starting with human stem cells, the researchers grew small, three-dimensional clumps of human tissue called organoids to model bronchial airway tissue, gas-exchanging “alveoli” tissue deep in the lungs, and heart muscle, all of which are known to be infectable by SARS-CoV-2.
In a high-level biosafety facility at NYU Grossman, the researchers exposed these organoids to different quantities of the virus and identified 18 genes that become consistently more active during infection, in multiple organoids and at different viral doses.
The scientists deleted these genes from the organoids, one by one, to see the effect on virus levels. The results suggested that while 13 of the genes appear to have some role in enabling SARS-CoV-2, so that virus levels are lower when they are absent, the strongest enabler by far was CIART. The latter encodes a transcription factor protein that normally works in the cell nucleus to regulate the activity of other genes. It had never before been linked to disease.
Further tests indicated that the CIART gene normally enhances the ability of SARS-CoV-2 to reproduce by boosting the production of certain fatty acids, via a pathway known as the RXR pathway. Treating the organoids with experimental RXR inhibitor compounds before exposure to SARS-CoV-2 effectively blocked the virus’s ability to establish infection in the tissues.
The findings suggest that targeting RXR or its upstream controller, the CIART protein, could be an effective way to treat SARS-CoV-2 infection, or even to prevent it over the short-term.
A big advantage of this approach, the researchers say, is that it alters the host side of the virus-host interaction.
“Most antiviral approaches to SARS-CoV-2 have focused on targeting some component of the virus itself, but the virus usually can evolve rapidly around that,” said Dr. Schwartz, who is also a hepatologist at NewYork-Presbyterian/Weill Cornell Medical Center. “It can be a lot harder for the virus to adapt to changes on the host side.”
The researchers now are continuing to study how CIART influences the viral life cycle—and how best to block its infection-enhancing effect.
Drs. Xuming Tang, research associate in surgery, Dongxiang Xue, postdoctoral associate in surgery, and Tuo Zhang, instructor in microbiology and immunology, at Weill Cornell Medicine, and Drs. Benjamin E. Nilsson-Payant and Lucia Carrau, a former and current postdoctoral associate at NYU Grossman School of Medicine, respectively, were co-first authors on the paper.
Many Weill Cornell Medicine physicians and scientists maintain relationships and collaborate with external organizations to foster scientific innovation and provide expert guidance. The institution makes these disclosures public to ensure transparency. For this information, see profile for Dr. Schwartz.