By Anne Machlinski
Illustration by Alexander Vidal
Photos by John Abbott
When Dr. Olorunseun Ogunwobi, an associate professor of biology at Hunter College and adjunct assistant professor at Weill Cornell Medicine needed African-American men to participate in his research on how genetics might play a role in prostate cancer disparities, he reached out to a well-known Bronx community leader to help him establish relationships with potential participants.

Illustration by Alexander Vidal
Building trust — as Dr. Ogunwobi plans to do by holding focus groups and information sessions with these men before he ever asks for the urine or tissue samples he’ll need to conduct his lab-based work — is essential, says Barbara Hart, executive director of the Bronx Health Link, an education, research and advocacy agency that works to improve health outcomes for residents of the borough. “We know how important it is for people in our community to participate in medical studies and to be part of the scientific research process from the very earliest stages — to share their needs and have their voices heard — to truly improve their health,” says Hart, noting that the borough is ranked last among New York State’s 62 counties when it comes to health indicators like asthma and diabetes rates, as well as maternal and infant mortality. “We want this partnership to last from start to finish — for researchers to come back and share what they find with us so that we can benefit from the results.” Because Dr. Ogunwobi’s approach includes a promise to return with clinically significant findings, Hart says she was happy to help him.

Dr. Julianne Imperato-McGinley.
While this interdisciplinary approach to medical research was once considered controversial because many senior scientists and physicians believed it would slow down the research process, today it’s clear that the NIH’s gamble paid off. The Clinical and Translational Science Center (CTSC) — which brings together Weill Cornell Medicine, Memorial Sloan Kettering Cancer Center, Hospital for Special Surgery, Hunter College’s Center for Translational and Basic Research, Animal Medical Center, Cornell Cooperative Extension’s New York City office, and the Ithaca campus’s School of Bioengineering and College of Veterinary Medicine, among other institutions — is one of more than 60 such federally backed programs nationwide. In the last decade, Weill Cornell Medicine’s CTSC has assisted at least 3,100 investigators, trained 1,200 early-career scientists, hosted 330 seminars and workshops, and partnered with 120 community organizations in areas of New York City where there are obvious health disparities and a special need for preventive services, such as the South Bronx; Jamaica, Queens; and Bushwick, Brooklyn. “I’m proud that we’ve been able to bring together these different institutions — each with their own culture and leadership — to work toward the same mission,” says Dr. Julianne Imperato-McGinley the CTSC’s founding director and principal investigator, Weill Cornell Medicine’s associate dean for translational research and education, and the Abby Rockefeller Mauzé Distinguished Professor of Endocrinology in Medicine. “CTSC-supported research now serves as an example of what successful interdisciplinary collaborations can accomplish.”Dr. Ogunwobi’s project — conducted in collaboration with Dr. Brian Robinson, MD ’06, an assistant professor of pathology and laboratory medicine at Weill Cornell Medicine, and Dr. Joseph Osborne, a radiologist at Memorial Sloan Kettering — is one of many supported by the Weill Cornell Medicine-led CTSC. This NIH-supported program, which began in 2007 with a $49 million grant (the largest federal grant ever made to Weill Cornell Medicine) that was renewed for the same amount in 2012, is part of a larger federal effort to support multi-institutional research consortiums that prioritize collaboration, mentorship and community participation to promote innovation and foster discoveries so that new treatments get to patients as quickly as possible.
These cross-institutional collaborations, which the CTSC funds with pilot grants of approximately $50,000 per year for up to two years, are the center’s cornerstone. Investigators from various disciplines and institutions use the money to work on innovative, high-risk pilot studies in which the outcome isn’t clear in advance. If the study goes well and investigators collect critical early findings to demonstrate why more research should be supported, they can apply to — and have a greater chance of receiving — external funding. That’s exactly how Dr. Michelle Bradbury, a professor of radiology in the Gerstner Sloan Kettering Graduate School of Biomedical Sciences, director of intraoperative imaging at Memorial Sloan Kettering Cancer Center and an associate professor of radiology at Weill Cornell Medicine, and Dr. Ulrich Wiesner the Spencer T. Olin Professor of Materials Science and Engineering at Cornell Ithaca, began their now decade-long collaboration.

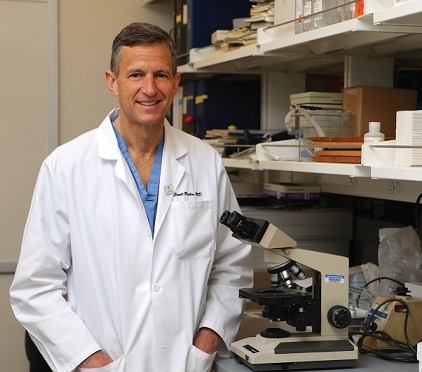
TEAM EFFORT: Collaborators on a CTSC-supported study of prostate cancer in African American men include WCM’s Dr. Brian Robinson (left), and MSK’s Dr. Joseph Osborne (right).
In 2007, Dr. Bradbury approached Dr. Wiesner about potentially working together to see if a tiny nanoparticle he’d developed, called Cornell dots (or “C dots”), could be used to detect cancer cells during imaging. Their early CTSC-funded research led to a larger NIH grant; from there they entered phase 1 clinical trials, formed a start-up company and launched, as co-directors, the $10 million, NIH-supported MSK -Cornell Center for the Translation of Cancer Nanomedicine. Today, they’re studying a newer generation of C dots that deliver drugs directly to tumors; eventually, Dr. Bradbury says, the technology could be used to both diagnose and treat various types of cancer. “Without that initial funding — which allowed us to explore the biology of the nanoparticle and figure out how to attach drugs to it — this would have been a much slower process,” she says. “The CTSC is responsible for getting this on the path to patients.”
Dr. Bradbury is now set to pay it forward. She has signed on to mentor early-career, CTSC-supported scientists, who are eligible to receive pre- or post-doctoral grants for interdisciplinary, translational research. “It’s really important that we actively engage with different levels of students and junior faculty,” Dr. Bradbury says, “because we understand what needs to be done to start a big translational research project and can help guide young people onto a successful path.” To achieve this same aim, the CTSC also invites anyone affiliated with a partner institution to take part in regular educational opportunities, including a master’s degree in translational research and day-long seminars on writing winning grants and publications or working with the FDA.
Mobile Applications
From the OR to the Lab and Back Again, Scientists Work to Improve a Common Knee Surgery
When it comes to the CTSC’s third core tenet — engaging with New Yorkers — Dr. Imperato-McGinley says she’s pleased with how far these relationships have come as the CTSC marks its 10-year anniversary. “Clinicians and scientists at Weill Cornell Medicine have always had a considerable responsibility to address health disparities that medically underserved, racial and ethnic minority populations face,” Dr. Imperato-McGinley says, “but before this grant came along, we weren’t working with communities as intensely as we needed to be.” Today, the center’s network of community leaders and local organizations — many of them faith-based — extends into the five boroughs. Physicians have screened thousands of residents in medically underserved areas at health-education and preventive-medicine events, both in person and through videoconferencing. And a few years ago, the CTSC started awarding $5,000 and $20,000 grants to support community leaders and researchers who are studying diabetes, depression, heart disease and other conditions that disproportionately affect disadvantaged New Yorkers. (Bronx Health Link’s Hart, who is also on the CTSC community advisory board, has received two awards.) Importantly, CTSC-supported investigators are now reaching out directly to underserved New Yorkers, asking for medical information to address their needs and to recruit them for minority-focused clinical research that bears on their health. “We’re finding creative ways to tackle the country’s biggest health problems, and are really going from the bench to the bedside and then into the community,” Dr. Imperato-McGinley says. “That’s as innovative as you can get.”
Mary Clare McCorry is an early-career scientist; she earned her master’s degree in biomedical engineering from Cornell Ithaca in 2015 and is set to complete her doctorate there in June, before embarking on a career of lab-based research. But as she looks back at her education, she says it was the summer spent observing knee surgeries that inspired her current line of investigation. “More than one million meniscus surgeries take place each year in the United States,” McCorry says of the trampoline-like structure that protects the knee’s cartilage and helps distribute weight. “But because the gold standard approach is to replace the meniscus with donor tissue from someone who was healthy, immuno-compatible, and about the same size as the patient receiving it, it’s nearly impossible to meet that demand.” Most of the time, McCorry says, surgeons just remove the injured part of the meniscus to reduce the pain, but don’t rebuild or replace it.
While this is workable in the short term, research shows that about ten to 15 years down the road, patients develop side effects like worsening knee pain, degeneration of the cartilage and arthritis. Since meniscus injuries typically happen in tandem with a tear to the anterior cruciate ligament, or ACL — common in sports like soccer, skiing and football — the patient is often young. In the worst-case scenario, they injure their meniscus at 15, have arthritis by 30, and undergo a total knee replacement (which only lasts a decade) soon after.
Dr. Scott Rodeo.
After observing numerous meniscus surgeries at Hospital for Special Surgery, McCorry began exploring how to create a tissue-engineered meniscus using stem cells and then anchor it in the body. She linked up with Dr. Lawrence Bonassar, an Ithaca-based professor of biomedical engineering, and Dr. Lisa Fortier, PhD ’99, a professor of large animal surgery at Cornell’s College of Veterinary Medicine, who contributed to the project’s design. Dr. Scott Rodeo MD ’89, the HSS orthopaedic surgeon and clinical scientist whom McCorry observed in the operating room, provided insights on how the tissue-engineered meniscus would work best in the people that need it.Offering early-career scientists the opportunity to collaborate with clinicians and investigators from different fields—and to see the power of translational research as they’re starting their careers — is essential, says Dr. Rodeo, who has worked with two trainees out of the 80 who have received grants from the CTSC to support their pre- and post-doctoral work. “There’s so much basic research done, but it doesn’t always get translated,” says Dr. Rodeo, also a professor of orthopaedic surgery at Weill Cornell Medicine. “This early exposure to the clinical side of things really fires up young investigators and gives them some context for what they’re doing, which is critical.”
During the project’s two-year term, which ended last year, the team figured out how to better engineer the artificial meniscus at its interface with the bone, and seed a mold with a culture of stem cells derived from both the meniscus and a patient’s bone marrow, which is easier for doctors to access. Dr. Bonassar plans to take these findings to apply for external funding. Eventually, the team hopes that a patient with an injured meniscus would get an MRI or CT scan from which investigators could generate a replica anatomical mold, which they’d seed with stem cells and implant in the body during surgery. Because it’s designed to grow and adapt to the patient’s anatomy, this tissue-engineered meniscus should reduce the risk of knee pain and arthritis later in life.
Next Generation
Dr. Evi Giannakakou Mentors Tomorrow’s Investigators
The CTSC has done more than fund Dr. Evi Giannakakou’s early investigations into how a blood test could be used to predict drug resistance in men with prostate cancer to better determine their care. It has also supported her efforts to help young scientists launch their careers. “The CTSC has been critical to the success of both of my main academic pursuits,” says Dr. Giannakakou, a professor of pharmacology at Weill Cornell Medicine and director of a program that helps early-career investigators apply for their first major grant. “It helped me and my collaborators collect preliminary data that allowed us to apply for larger federal opportunities, and got a much-needed program off the ground.”
The research that the CTSC supported back in 2008 involves a collaboration between Dr. Giannakakou and Dr. David Nanus, the Mark W. Pasmantier Professor of Hematology and Oncology in Medicine at Weill Cornell Medicine and chief of hematology and medical oncology at NewYork-Presbyterian/Weill Cornell Medical Center, as well as Dr. Brian Kirby, a professor of mechanical and aerospace engineering at Cornell Ithaca. The trio teamed up about a decade ago, when Dr. Kirby presented his work in microfluidics at a cross-campus symposium meant to spur collaborations. Soon after, Dr. Giannakakou and Dr. Nanus approached him to see if he’d be willing to design a device that could isolate circulating tumor cells in blood samples collected from men with prostate cancer. They explained that while the standard of care for prostate cancer patients was either chemotherapy or hormone-based therapies, there was no adequate way to determine which treatment would work for individual patients. Their hope was that by studying genetic markers from the circulating tumor cells, they could help clinicians customize therapies soon after their patients are diagnosed.
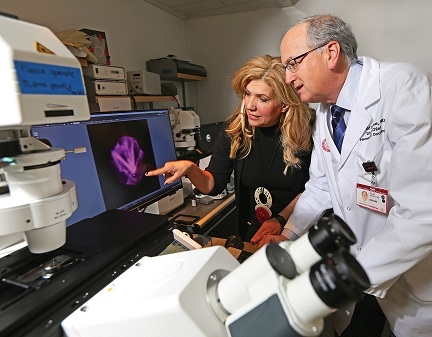
Dr. Evi Giannakakou(left), and Dr. David Nanus.
Dr. Kirby agreed to join forces, and today, blood-based liquid biopsies like the one Dr. Giannakakou and Dr. Nanus first proposed have had a huge benefit on the field. “This research allows you to obtain tumor information from the patient as often as you like, with a simple blood draw,” Dr. Giannakakou says. “In addition, while the information you receive from a traditional tissue biopsy is limited by the location from which the cells were removed, circulating tumor cells tell a more complete story about the entire progression of disease throughout the body.” Dr. Giannakakou is now using this approach to help explain why prostate cancer cells often become resistant to standard therapies over time, and along with Dr. Kirby has adapted the technology to ultimately study circulating tumor cells in cancers of the lung, breast and gastric system.
Dr. Giannakakou is simultaneously doubling down on her mentorship efforts. In fall 2015, she started a program modeled after a Harvard CTSC initiative that prepares junior investigators to apply for the NIH’s oldest and most commonly used grant, the R01. The Weill Cornell Medicine CTSC sponsored the program and contributed $20,000 to get it off the ground, and Dr. Giannakakou notes that it has had a remarkable success rate — 50 percent — in applications that have received federal funding. “The CTSC was critical to its success,” she says, “and I will forever be grateful for that.”
This story first appeared in Weill Cornell Medicine, Vol. 16. No. 2

