A naturally produced chemical exacerbates infection by a common bacteria, rendering the infection significantly harder for the body to clear, according to new research from Weill Cornell Medicine and Cornell University. The bacteria, Pseudomonas aeruginosa, is especially harmful for patients with the lung disease cystic fibrosis; investigators hope this understanding will help facilitate the development of improved therapies.
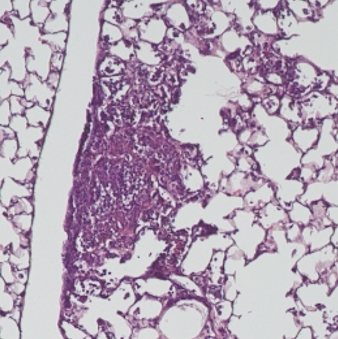
Inflamed area of a lung infected with Pseudomonas combined with 2,3-butanediol. Image credit: Worgall Lab.
The pre-clinical findings, published May 13 in the ISME Journal, explore the relationship between 2,3-butanediol, a chemical produced by the bacteria that naturally live in the lungs, and P. aeruginosa, a common bacteria that healthy patients clear easily but that stubbornly remains in cystic fibrosis patients, causing increased inflammation. The interaction between the two components, the study shows, yields an infection far more harmful than P. aeruginosa would create alone.
"It’s always been a big mystery why patients with cystic fibrosis do so poorly once they have P. aeruginosa in the lung. Our findings show that we not only have to look at the bacteria itself, but we also have to look at the interaction of the natural bacteria in the lung," said Dr. Stefan Worgall, distinguished professor of pediatric pulmonology and a professor of pediatrics and genetic medicine at Weill Cornell Medicine.
Scientists from Weill Cornell Medicine and Cornell University collaborated on the research, infecting a group of mice with P. aeruginosa and another with P. aeruginosa combined with 2,3-butanediol. After three days, the mice with both factors had more than 100 times more of the bacteria in their lungs. The inability to eradicate the 2,3-butanediol-laden bacteria suggests why P. aeruginosa has posed such a significant problem for cystic fibrosis patients.
The findings also demonstrate that a concoction of naturally occurring bacteria, known as a microbiome, exists in the respiratory tract — and that it can play an important role in influencing health.
Currently, cystic fibrosis patients take antibiotics continually if they are diagnosed with the infection; however, the lengthy treatment is not always effective. The investigators hope their findings will lead to advances in keeping cystic fibrosis patients protected against infection.
"We need to understand the disease process better, and how this infection settles in the lung and interacts with the microbiome," said Dr. Largus Angenent, a professor of biological and environmental engineering at Cornell University who co-directed the research. "That understanding is what will eventually lead to new therapies."
