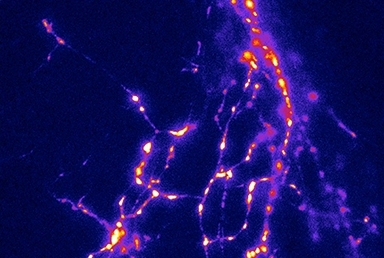
Fluorescence signals from vGlut1- pHluorin, a synaptic vesicle exocytosis biosensor, expressed in rat hippocampal neurons after electrical stimulation. Image credit: Drs. Hugh Hemmings, Zhenyu Zhou and Daniel Cook
One of the most commonly used general anesthetics induces unconsciousness in part by reducing the amount of calcium ion that flows into nerve cells and triggers chemical communication between them, a team of Weill Cornell Medicine investigators show in new research. The findings shed light on how anesthetics work, and may lead to the safer use of current agents or the development of better agents that are just as effective but carry fewer side effects.
General anesthesia is widely considered to be one of the most important advances in medicine. The ability to induce a pain-free, unconscious state in patients has allowed physicians to perform surgeries and procedures that would not be possible in a conscious patient. While anesthetics have been in wide use for more than a century, little is known about how exactly they work in the brain to block sensation and induce unconsciousness. General anesthetics can also cause serious side effects, ranging from breathing and heart rate changes during surgery to nausea and vomiting post-operatively, and even decreased mental function or mood changes for several days after anesthesia. Much of anesthesia research is focused on understanding how such drugs affect cells in the brain, so that researchers might refine them to increase effectiveness and avoid troublesome side effects.
"We need to know more about how these drugs work so that we can use them more insightfully and maybe even make safer versions of them," said Dr. Hugh Hemmings, Jr., chair of the Department of Anesthesiology at Weill Cornell Medicine.
Scientists have long understood that anesthesia affects communication between nerve cells, or neurons. Now, in their study, published in the Sept. 9 issue of the Proceedings of the National Academy of Sciences, Dr. Hemmings and his colleagues at Weill Cornell Medicine, Dartmouth College and Kurume University School of Medicine in Japan discovered where in the brain this happens.
The investigators found that the general anesthetic isoflurane, a commonly used derivative of ether, inhibits cell-to-cell communication by reducing the amount of calcium ion that flows into nerve cells. Calcium ion provides the signal for neurons to communicate with each other through the release of chemical neurotransmitters; reduced calcium ion influx results in reduced cellular communication, which contributes to anesthesia's characteristic unconsciousness and lack of movement in response to pain.
For their research, the investigators placed fluorescent biosensors into neurons cultured from rats. This allowed the scientists to visualize the fusion of synaptic vesicles, small packets containing neurotransmitter, from the axon terminals of neurons when anesthetic was administered. They also measured the amount of calcium ion that flowed into the cells in the presence of isoflurane.
"We found that isoflurane inhibited calcium entry into the cells," said Dr. Hemmings, the Joseph F. Artusio, Jr. Professor of Anesthesiology and a professor of anesthesiology and of pharmacology, who is the study's senior author. In addition, there was a proportional amount of reduced communication between neurons. "This tells us that the effect of anesthetics is through some target that inhibits calcium entry into the neuron," he added.
Ultimately, if that target can be identified, anesthetics could be engineered to be more clinically effective and have fewer side effects, Dr. Hemmings said.
Co-authors on the study included Drs. Joel P. Baumgart , Zhenyu Zhou , Masato Hara, Daniel C. Cook '15, Michael B. Hoppa , and Timothy A. Ryan.
