With a radical new prosthetic retina, Sheila Nirenberg, PhD, aims to help millions with degenerative eye disease
Some 10 million Americans have degenerative retinal disease; of those, 1.9 million suffer from advanced-stage blindness. Historically, there has been little that doctors can do. Medications help only a small subset of patients — and then just slightly improve vision or slow the disease's progress. So far, prosthetic retinas have had limited appeal: They reveal high-contrast edges and spots of light, allowing people to orient themselves within spaces they already know but hardly approximating normal vision. But now an experimental, next-generation artificial retina developed by Sheila Nirenberg, PhD — associate professor of computational neuroscience in the HRH Prince Alwaleed Bin Talal Bin Abdulaziz Alsaud Institute for Computational Biomedicine and in the Department of Physiology and Biophysics — is currently in the animal testing phase and showing great promise, producing images so sharp and subtle that they closely resemble what a fully sighted person would see.
In healthy eyes, the retina serves as the entryway for visual information to travel to the brain. At its front end, photoreceptors pick up patterns of light and dark. In the middle, complicated circuitry extracts information from those patterns, "converting it into a code the brain can read," Nirenberg explains. From there, the retina's ganglion cells send that neural code to the brain in the form of electrical signals called spikes. Any image can be converted into its own corresponding code, or pattern of spikes, using a set of mathematical equations.
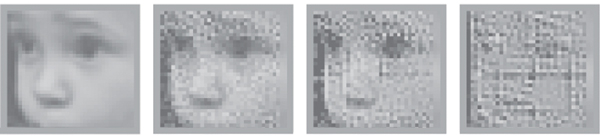
In sight: An image of a child's face seen in its original form (A), as it has been encoded by the new prostethic device (B), and how it is reconstructed from those signals and "seen" by the patient (C). D shows the same image reconstructed from the signals of a blind retina treated with the standard prosthetic.
Existing artificial retinas, which have been around for about two decades, have tried to replicate the work of the photoreceptors with surgically implanted, light-receiving electrodes. But without incorporating the neural code to decipher what's in front of the eye, Nirenberg says, "they're very limited — it's nothing close to normal vision." She and postdoc Chethan Pandarinath, who earned a PhD in Nirenberg's lab, have taken a different, two-pronged tack: a device that processes the code plus gene therapy that activates the ganglion cells.
Surgically implanted electrodes are not the main focus of Nirenberg's design. Instead, a patient would receive gene therapy that makes the ganglion cells — which are typically spared by retinal diseases — express a light-sensitive protein called channelrhodopsin. "Surgery won't need to be involved," Nirenberg says, "just a quick injection into the eye." About three weeks later, after the therapy has taken hold, a patient would don glasses containing a camera and a chip (similar to the microprocessors inside cellphones) that processes the code. The camera "sees" the images and sends them to the chip, which converts them to light pulses. Those pulses are actually image-specific neural code, and they activate the light-sensitive channelrhodopsin in the ganglion cells. In so doing, the cells can fire the right code to the brain so the patient can see. "Other people have also used this light-sensitive gene, but they don't have the retina's code, which is our key ingredient," Nirenberg notes. "We've brought it back to life so it can fire like a normal retina."
Until she began testing the artificial retina, Nirenberg's focus was largely on basic science, focusing on two fundamental conceptual challenges in neuroscience: understanding the neural code and determining how populations of retinal neurons work together to encode scenes such as faces and landscapes. In 2009, one of her students mentioned improvements in channelrhodopsin technology — and Nirenberg had a eureka moment. "I thought, Wow, now we can put our knowledge of the code with channelrhodopsin and this will work," she remembers. "I almost fell off my chair. I realized I knew exactly how to make a prosthetic."
When Nirenberg and Pandarinath tested the concept in mice later that year, it worked as anticipated. In findings she presented at last year's Society for Neuroscience meeting, Nirenberg showed that the retinas of completely blind mice were able to produce normal firing patterns and animals treated with the technology could discern moving images. The results led to a $250,000 prize from the BioAccelerate NYC contest to develop the technology for commercial use. Nirenberg plans to collaborate with scientists from Harvard, the University of Florida, and a German company to develop it for monkeys — and, ultimately, people. "It's exciting to know that what you've been working on suddenly has human value," Nirenberg says of her shift from basic science to clinical applications, "especially as the years go by and you realize you need to do something for people, not just because it's intellectually interesting." Tests of the retina in monkeys have begun, and if all goes well, it could be on the market within five years, Nirenberg says. The coding aspect of the technology could also be used to drive the electrodes in patients with older prosthetic retinas.
If the device sounds like science fiction, Nirenberg says, its results would be unmistakably real to the people who receive it. She admits that patients wearing the glasses might "look sort of dorky." But the ultimate hope, she says, is that "they'd be able to see — see patterned images, see faces, walk through the supermarket and pick out a box of cereal, recognize their children."

