The study of human pluripotent stem cells, which can develop into any cell type in the body, is providing Weill Cornell Medicine and NewYork-Presbyterian investigators with new insights into the virus that causes COVID-19 and how it may infect organs such as the pancreas and liver.
The study, published June 19 in Cell Stem Cell, demonstrates that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can infect endocrine cells in the pancreas, which supports other emerging evidence that COVID-19 is strongly associated with type 2 diabetes.
“It was a bit surprising that the pancreatic endocrine cells can be infected by SARS-CoV-2,” said lead study author Dr. Shuibing Chen, an associate professor of chemical biology in surgery and of chemical biology in biochemistry at Weill Cornell Medicine.
Dr. Shuibing Chen
Pancreatic endocrine cells are responsible for producing hormones such as insulin and glucagon, which help balance the body’s blood sugar levels. When the pancreas doesn’t work properly, diabetes can develop.
While recent clinical data demonstrate poor outcomes in people with pre-existing diabetes and COVID-19, the new finding reflects growing evidence that COVID-19 may also be responsible for new-onset diabetes. “The relationship between diabetes and COVID-19 appears to be bidirectional,” said Dr. Chen, adding that this is an area for further study.
The researchers also discovered that the liver may be susceptible to SARS-CoV-2 infection. Clinical evidence is emerging that liver damage can occur in COVID-19 patients, even though other coronaviruses have not been thought to infect this organ.
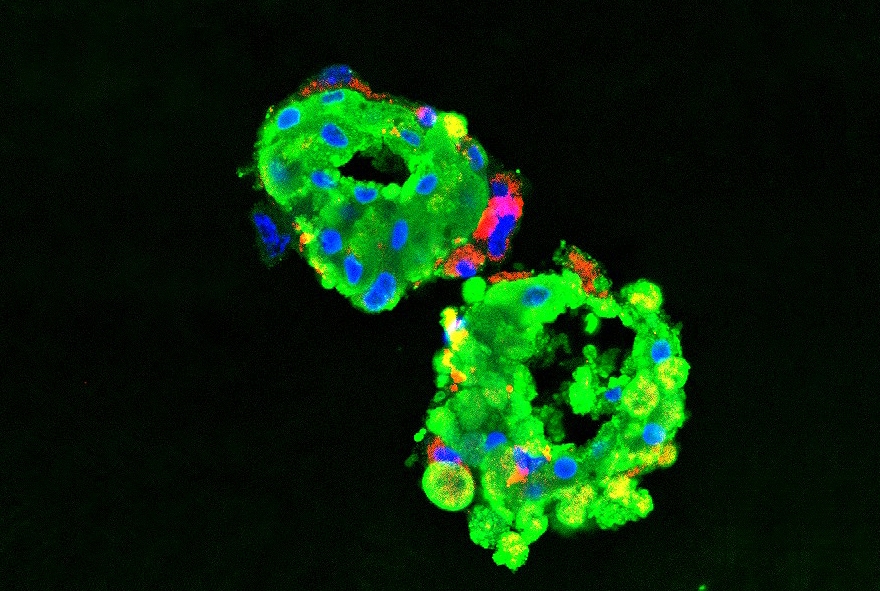
Dr. Chen and her colleagues decided to use a pluripotent stem cell model to study COVID-19 because it allows scientists to create cell types and mini-organs, or organoids, that are closer to human tissue than other common laboratory models.
Traditionally, viruses are studied using a variety of different cell lines generated from cancer cells, said study co-author Dr. Robert Schwartz, assistant professor of medicine at Weill Cornell Medicine and an attending physician at New York-Presbyterian/Weill Cornell Medical Center. However, these cell lines don’t accurately represent the organs that researchers are trying to model, including the pancreas and the liver.

Dr. Robert Schwartz
“Pluripotent stem cells give us the ability to generate cells that comprise specific organs in a way that is physiologically relevant,” said Dr. Schwartz. “Everything we're looking at is human, which adds a lot of strength to our data. We could try to do this in a mouse, but that has its own inherent challenges.”
For the current paper, the researchers studied liver organoids and several other cell types, including: pancreatic endocrine cells; endothelial cells, which line the blood vessels; cardiomyocytes, which make up the heart tissue; macrophages, or large white blood cells important to the immune system; microglia, which are responsible for the immune response in the central nervous system; cortical neurons, which transmit information in the brain; and dopaminergic neurons, which produce the chemical dopamine in the central nervous system.
The researchers then determined whether these cell types and organoids expressed angiotensin-converting enzyme 2 (ACE2), a protein receptor that sits on the surface of cells. “Scientists think this receptor acts like a gateway for SARS-CoV-2 to enter the cell, causing infection,” Dr. Chen said.
They found that pancreatic endocrine cells and liver organoids readily expressed ACE2, as did endothelial cells, cardiomyocytes, microglia, macrophages, and dopaminergic neurons. Cortical neurons expressed ACE2 at lower levels.
The researchers then introduced a pseudovirus, meaning a modified form of SARS-CoV-2 that is safer to work with but that can mimic its infectious activity, to determine how readily the organoids and cell types can be infected. Pancreatic endocrine cells, liver organoids, cardiomyocytes, and dopaminergic neurons were easily infected, while infection did not occur as readily in endothelial cells, microglia, macrophages, or cortical neurons.
ACE2 expression did not seem to be sufficient for infection of macrophages or cortical neurons, a finding that the researchers will further explore, said Dr. Chen. While a lot of drug development is currently focused on targeting the ACE2 receptor, “there may be additional components that are critical to infection that are yet to be discovered,” she said.
To further demonstrate the strength of their pluripotent stem cell model, the researchers studied chemokine response in their cell types and organoids. Chemokines attract white blood cells to the site of infection, creating an inflammatory response in the body. The cells and organoids showed similar chemokine responses as lung autopsy tissue samples from COVID-19 patients. “This finding further suggests that our model really captures what happened in the human patients,” said Dr. Chen.
The researchers also plan to further study the impact of SARS-CoV-2 on cardiomyocytes, because cardiac involvement is a common feature in hospitalized COVID-19 patients and is associated with poor prognosis. “We hope to expand our pluripotent stem cell model so we can start looking for some small molecules or drug candidates that can protect the hearts of COVID-19 patients,” said Dr. Chen.

Dr. Todd Evans
“The COVID-19 crisis inspired a diverse group of investigators to work together under difficult circumstances and collaborate across multiple disciplines to develop a novel platform for modeling this new human disease,” said co-author Dr. Todd Evans, the Peter I. Pressman M.D. Professor of Surgery and associate dean for research at Weill Cornell Medicine. “The team’s plan to use the pluripotent stem cell platform to screen drugs that block SARS-Cov-2 activity in multiple human cell types is already showing promise and provides a paradigm shift for drug discovery,” said Dr. Evans.
A robust testing platform that has some fidelity to the actual SARS-CoV-2 infection may mean that “studies evaluating existing drugs to treat COVID-19 will have a greater potential for success,” said Dr. Schwartz.