Weill Cornell Medicine researchers and the TB Drug Accelerator have received two grants totaling $6.8 million from the Bill & Melinda Gates Foundation to study tuberculosis (TB) drug development. This effort will expediate finding new drug targets within the bacteria and identifying new lead compounds, two significant bottlenecks in TB drug development.
“These grants allow us to apply the assays we’ve developed in the last few years, focusing on the most promising targets for TB drug development,” said principal investigator Dr. Dirk Schnappinger, professor of microbiology and immunology at Weill Cornell Medicine and a member of the TB Drug Accelerator.
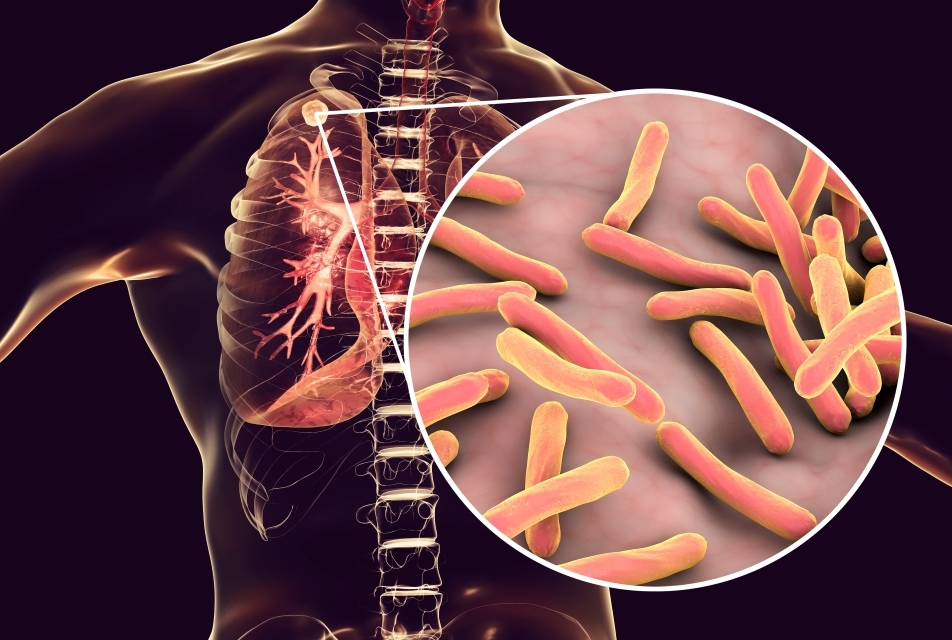
Mycobacterium tuberculosis (Mtb), bacteria that infect and multiply in the lungs, cause cough, fever and chest pain. Highly contagious, TB remains one of the most devastating infectious diseases. Last year, 10.6 million developed the condition globally, resulting in approximately 1.3 million deaths, according to the World Health Organization.
Dr. Dirk Schnappinger
TB treatment requires taking several antibiotics for up to nine months. “We could treat TB much better in the regions where the disease takes its biggest toll, if we could shorten the time patients need to take antibiotics and discover more effective medications,” Dr. Schnappinger said.
One of the reasons it is difficult to eliminate Mtb is its ability to adapt to different conditions inside the human body, allowing it to evade treatment through drug resistance and drug tolerance. Drug resistance forms when spontaneous gene mutations render the bacteria resistant to commonly used TB drugs, usually when patients fail to complete the treatment regimens. Drug tolerance occurs when the bacteria undergo a physiological change that allows them to escape treatment that would normally kill them.
Looking for New Small Molecule Drugs
One of Dr. Schnappinger’s research goals is to prioritize the small molecules that have been identified by other members of the TB Drug Accelerator for further development. His team is using genetic methods to probe how these small molecules can kill or inhibit the growth of Mtb. Ideally, discovering several molecules that work in different ways would help combat drug resistance.
The small molecules are tested on Mtb mutant libraries containing 30,000 to 100,000 strains generated in collaboration with Dr. Jeremy Rock, head of the Laboratory of Host-Pathogen Biology at Rockefeller University. Each bacterial strain has a different gene underexpressed so less of that protein is produced. When a small molecule eliminates or inhibits the growth of a particular Mtb strain, the researchers can identify the underexpressed gene as the bacteria’s weak point.
Another approach is testing the small molecules on an Mtb overexpression library, which consists of about 1,000 Mtb strains, each designed to produce too much of an essential gene product. A small molecule would stop inhibiting the growth of a strain, if its target is overexpressed. “Profiling small molecules with both knockdown and overexpression libraries allows us to better predict the direct target of a small molecule,” he said.
Furthermore, the researchers are isolating Mtb mutants that are resistant to the small molecules being studied to understand how mutations render the bacteria impervious to the drug.
This multi-prong approach is shedding light on how the small molecules of interest inhibit growth of Mtb, their potential toxicities and suggest other structurally related molecules that may be more effective. Taken together the information is helping researchers prioritize which compounds to move forward for drug development.
Decreasing Treatment Time
The second grant is supporting efforts to shorten TB treatment time. Current drugs were developed to inhibit growing Mtb, so unsurprisingly, these drugs do not work as well for Mtb strains that are not growing or dormant. For example, granulomas, a hallmark of TB, are clusters of white blood cells with a center of dying cells. The bacteria inside the granuloma often stop growing and resist current drug treatments, which likely contributes to the long time needed to cure patients. “Identifying drugs that are more effective against this Mtb population is expected to shorten treatment,” he said.
This research aims to identify drug targets that are critical for survival of Mtb during infections, including within the center of granulomas and drug tolerance. Drugs designed against these targets may work faster and suggest viable combination treatments.
Such ambitious work has benefited from the collaborative effort of Weill Cornell Medicine researchers, said Dr. Schnappinger. They include Dr. Sabine Ehrt, professor of microbiology and immunology and co-chair of the immunology and microbial pathogenesis graduate program; Dr. Carl F. Nathan, chair of microbiology and immunology; Dr. Kyu Y. Rhee, professor of microbiology and immunology and professor of medicine. Dr. Michael Glickman at the Sloan Kettering Institute also contributed to this effort.
“One of our main goals is to extend this work to TB animal models, which will allow us to evaluate drug targets in the context of an infection,” Dr. Schnappinger said. “Ultimately, we want to find the Achilles heel of this pathogen.”