By Syl Kacapyr
Researchers from the Meinig School of Biomedical Engineering and Weill Cornell Medicine are teaming up to learn more about antibiotic resistance in neutropenic patients — individuals with low levels of infection-fighting white blood cells, such as those with leukemia.
The research project is funded with a $500,000 grant from the Centers for Disease Control and Prevention, which is leading a national initiative to combat drug-resistant organisms, sometimes referred to as "superbugs."
Leukemia patients produce abnormal white blood cells, resulting in fewer cells that are able to ward off harmful bacteria that can cause infections. Treatments such as chemotherapy and hematopoietic stem cell transplants further compromise the immune system. This forces patients to rely heavily on antibiotics to fight infection and sepsis, according to Dr. Ilana Brito, assistant professor of biomedical engineering and co-investigator of the project.
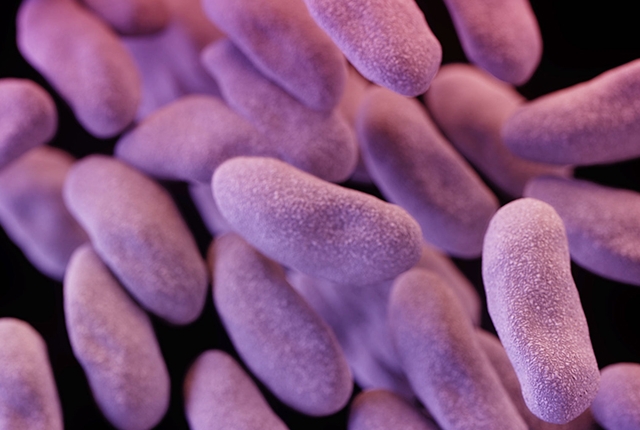
"They remain hospitalized for about one month and are therefore highly susceptible to hospital-acquired antibiotic-resistant infections, such as carbapenem-resistant Enterobacteriaceae (CRE), which can be life-threatening," Dr. Brito said.
Those patients can then carry the drug-resistant bacteria and spread it to other people, especially those who have a disrupted microbiome. CRE is one of the most concerning antibiotic infections that is transmitted. A 2013 study found that most patients hospitalized because of CRE received it from either a long-term care facility or another hospital.
Dr. Brito and co-investigator Dr. Michael Satlin of Weill Cornell Medicine's Transplantation-Oncology Infectious Diseases Program in the Division of Infectious Diseases, will examine antibiotic-resistance genes in neutropenic patients, changes in their microbiomes and their susceptibility to infection.
"Most of the infections in these patients are from gut bacteria," said Dr. Satlin, an assistant professor of medicine at Weill Cornell Medicine. "This project will allow us to understand how genes that confer resistance to important antibiotics spread among gut bacteria and proliferate in the setting of antibiotic exposures. A better understanding of resistance in the gut microbiome of these patients, and the effect that antibiotics have, could lead to new strategies for preventing and treating infections in this vulnerable patient population."
Dr. Satlin's previous work examined the growing threat of multidrug-resistant infections, including CRE infections in organ transplant recipients and patients with hematologic malignancies. Dr. Brito has studied the mobile genes that play a role in the human microbiome and can transfer between organisms. Earlier this year she published a first-of-its-kind study of native Fijian islanders, producing the first metagenomic view of the microbiome in the developing world.
To help scientists learn more about antibiotic resistance and the human microbiome, the U.S. Congress appropriated $160 million in its Fiscal Year 2016 budget to fund related research. The call for solutions reached the world stage in September when members of the United Nations General Assembly formally committed to fighting antimicrobial resistance together.
"To protect people, their microbiomes and the effectiveness of antibiotics, this project is an example of applied research that has the potential to produce innovative public health approaches to better combat antibiotic resistance," said Clifford McDonald, associate director of science for the CDC's Division of Healthcare Quality Promotion.
A version of this story first appeared in the Cornell Chronicle.
Syl Kacapyr is public relations and content manager for the College of Engineering.