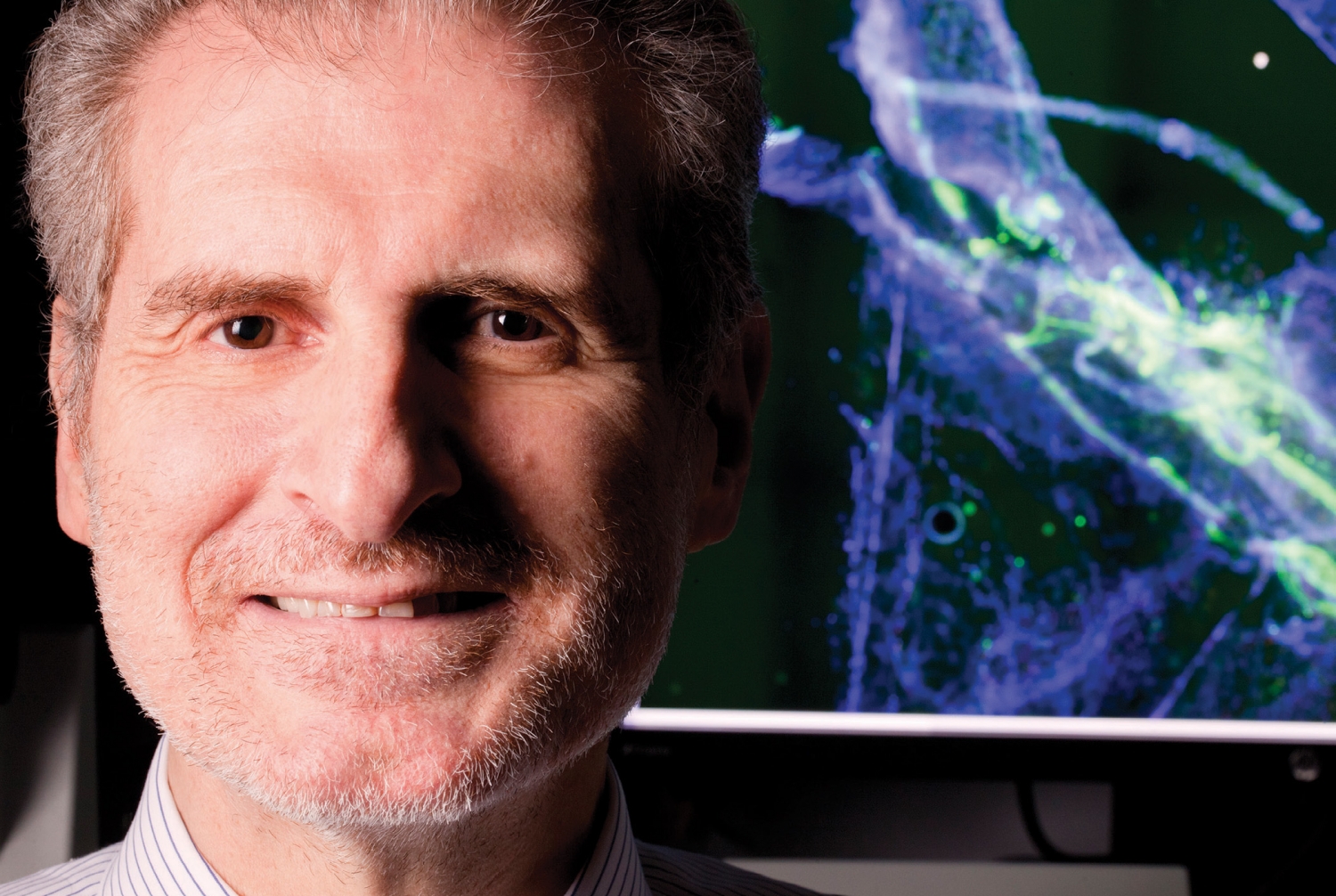
Dr. Costantino Iadecola has long been at the vanguard of understanding the vascular drivers of Alzheimer's disease
Today Dr. Costantino Iadecola is known as one of the world's leading experts on dementia, stroke and the aging brain. Twenty-five years ago, he was considered something of a heretic.
In the early '90s, Dr. Iadecola's team at the University of Minnesota Medical School discovered that mice genetically engineered to get Alzheimer's disease also developed blocked vessels in their brains, reducing cerebral blood flow by as much as 30 percent. This occurred before a mouse showed any signs of dementia, but it was clearly connected to the severity of the animal's eventual symptoms. At the time, scientists were aware that plaques, made up of accumulations of the peptide amyloid beta, played a major role in Alzheimer's. But they believed that it was a disease of the neurons, not of the brain's vascular system. "Nobody thought blood vessels were relevant," says Dr. Iadecola, now the director of the Feil Family Brain and Mind Research Institute and the Anne Parrish Titzell Professor of Neurology at Weill Cornell Medicine. "Obviously, the Alzheimer's field was skeptical."
By 2000, epidemiological and pathological data had caught up: It was clear that people with Alzheimer's also had suffered damage to the brain's blood vessels, including blockages that caused small strokes. The two most common types of dementia — Alzheimer's and vascular dementia, caused by small strokes — were connected. "Eventually the field came around," Dr. Iadecola says. "Everybody confirmed the other results, and new data showed there was a reduction in blood flow even before a patient displayed the first signs of cognitive impairment. Now it has become common knowledge, and there is a major push at the level of governmental funding agencies to investigate the vascular components of dementia."
That push includes a five-year, $2 million grant from the National Institutes of Health, awarded to Dr. Iadecola's longtime collaborator Dr. Chris Schaffer, an associate professor of biomedical engineering on the Ithaca campus and of neuroscience in the Feil Family Brain and Mind Research Institute. A physicist by training, Dr. Schaffer specializes in developing novel, optics-based tools and techniques for biomedical research. "He is a world leader in this new technology," Dr. Iadecola says. "It's cutting edge, using lasers to image the brain and to do all kinds of experiments that were not previously possible."
The grant will fund Drs. Schaffer and Iadecola's continuing investigations into the impact of blood-flow disruptions on the course of Alzheimer's disease. During a previous study, they noticed that Alzheimer's mice were experiencing a slowing of blood flow at the level of individual capillaries ("which could cause the smallest stroke you could imagine," Dr. Schaffer says). When they looked more closely at these tiny occlusions, they realized that they might have discovered the key to the relationship between reduced blood-flow to the brain and the amyloid beta plaques that were the hallmark of Alzheimer's disease. "In essence, what Chris and his team found was that, in the smallest possible vessels in the brain — capillaries — there were white blood cells blocking blood flow or making the flow sluggish," Dr. Iadecola says. "Now, this puts in a new twist to the whole story, suggesting that there may be something happening within the plumbing itself that prevents the normal flow of blood that the brain desperately needs to keep working." Essentially, the brain's drains get blocked, launching a vicious cycle in which amyloid beta — normally cleared out of the brain before it can accumulate — is allowed to build up and form neurotoxic plaques. "You decrease the clearance, and the concentration is higher," Dr. Schaffer says. "The concentration gets higher, then the probability of aggregation is higher. And the aggregates of amyloid beta drive the inflammation, which causes decreased brain blood flow."
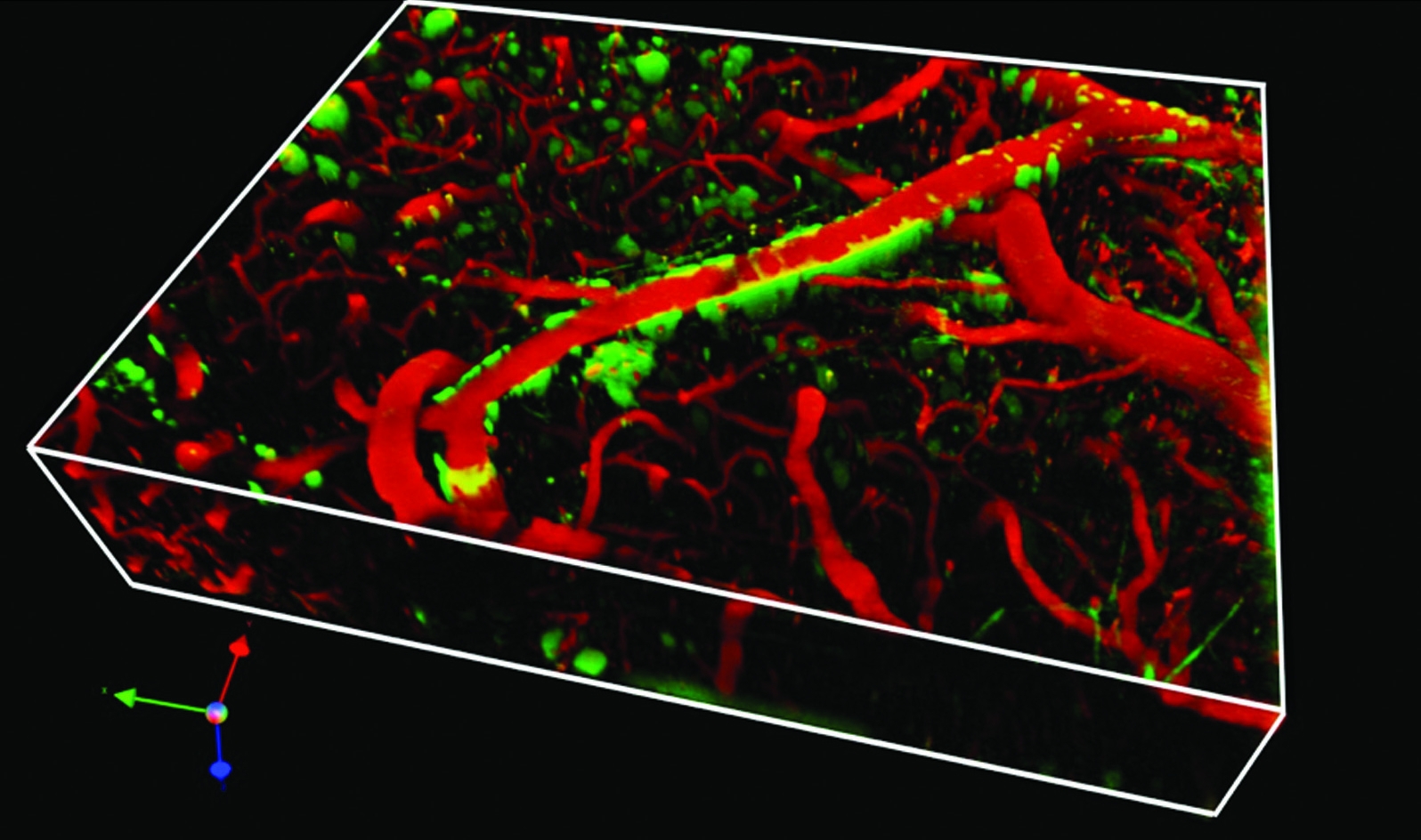
Mind and matter: Blood vessels in a mouse brain (seen in red) surrounded by amyloid plaque (green) Photo credit: Dr. Chris Schaffer
The pair's research could point to new targets for drugs that could slow or even stop the progress of the disease, and they are now trying to understand the molecular signaling that makes white blood cells adhere to the inside of the brain's capillaries in the first place. But their findings also reinforce the importance of maintaining good cardiovascular health — not only to prevent heart attack, stroke and other well-known consequences of atherosclerosis and high blood pressure, but to stave off dementia.
The good news, Dr. Iadecola says, is that thanks to several years of messages about maintaining vascular health, the rate of Alzheimer's seems to be going down; though in the aging global population the number of patients with dementia will continue to increase, it will be at a slower rate. "In the absence of a cure, there is now, in the United States and in the world, a much greater appreciation for preventing Alzheimer's disease," he says. "And this means controlling vascular risk factors like hypertension, diabetes, cholesterol, lack of mobility, smoking — all the things that make the vessels suffer." Dr. Iadecola notes that the involvement of the brain's vascular system could also help explain why mental agility exercises and learning new things seem to buffer against Alzheimer's: Mental activity increases blood flow. "Whether you're learning a new language or a musical instrument," he says, "You should always keep your brain active to keep Alzheimer's away."
— Amy Crawford
This story first appeared in Weill Cornell Medicine, Vol. 15, No.1.