Tissue engineers at Weill Cornell Medical College have created replacement body tissue with built-in blood vessels, an advance that overcomes one of the most difficult problems in the field: getting an immediate and adequate blood supply to human-engineered tissues as soon as they are transplanted into the patient.
"The major challenge is and has always been the ability to make things which have their own blood supply," said Dr. Jason Spector, an associate professor of surgery (plastic surgery) and otolaryngology at Weill Cornell. "Anything that is tissue engineered is severely limited without a blood supply."
The problem is particularly troublesome in exactly the kinds of patients who often need replacement tissue – patients who have health problems such as diabetes or cancer or those with infected or radiated wounds, which all slow the natural healing process.
Dr. Spector's technique, which was published April 8 in Tissue Engineering, takes a common connective tissue used in tissue engineering—type I collagen—and then fills it with strings of "sacrificial fibers" that create a 3-D network of very small channels, similar to networks of the body's smallest blood vessels.
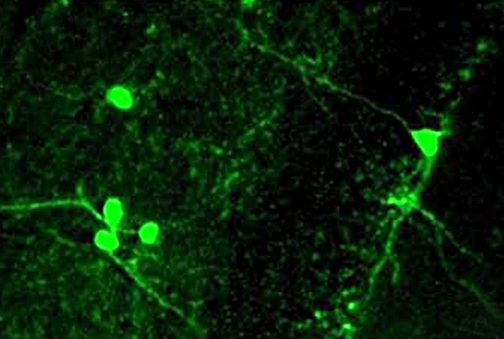
The "sacrificial fibers" are then dissolved away, leaving a network of hollow microchannels that are seeded with the cellular building blocks of blood vessels. Over time, these seeds grow to create fully formed blood vessels. Although other groups have designed engineered tissues containing vessels, none of those were built to be immediately connected to the host vascular system, which is crucial for the survival of cells within the construct of engineered tissue.
"That's a major leap forward, at least in terms of what I consider the holy grail of tissue engineering—making tissue-engineered constructs that not only contain their own vasculature, but that we as surgeons can use clinically," Dr. Spector said.
In the Tissue Engineering paper, Dr. Spector's group demonstrated that is it possible to attach an existing blood vessel to their engineered blood vessel within the construct. The technique immediately filled the man-made replacement tissue with blood and the blood flow lasted several hours.
Dr. Spector said that the potential clinical applications are far-reaching. In the near future, the engineered tissue could be used in the early stages of drug development to test new compounds in "living" tissue, rather than in petri dishes of cells. It also could be used to study the way cancerous cells interact with healthy tissue in three- dimensional environments. Next up would be using the tissue in large skin grafts.
Ultimately, Dr. Spector believes these engineered tissues could be used as a platform to artificially grow any kind of tissue found in the human body.