Scientists are closing in on a common dysfunction that appears to underlie a majority of severe brain injuries, raising real hope that many affected patients, even those with very limited apparent consciousness, could be helped with treatment.
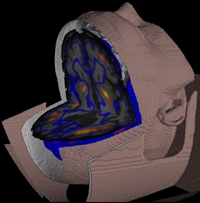
This rendering shows a common pattern of metabolic activity in a severely brain-injured patient. Weill Cornell scientists found the same pattern of low activity in 24 patients, no matter how they were hurt, pointing to a new way to assess such patients for possible cognitive reserve and treatment. Image: Schiff Lab
The study, led by Weill Cornell Medical College investigators and reported in PNAS, demonstrated the same pattern of low activity in a crucial brain circuit in 24 severely brain injured patients — no matter how their brains were injured — compared to 10 healthy participants.
Given that investigators showed in a recent study that the brains of several patients with similar patterns of altered activity could be switched on with the use of the sleep drug Ambien, patients like those in the new study may be candidates for Ambien or other drugs that activate that neural circuit, the scientists say.
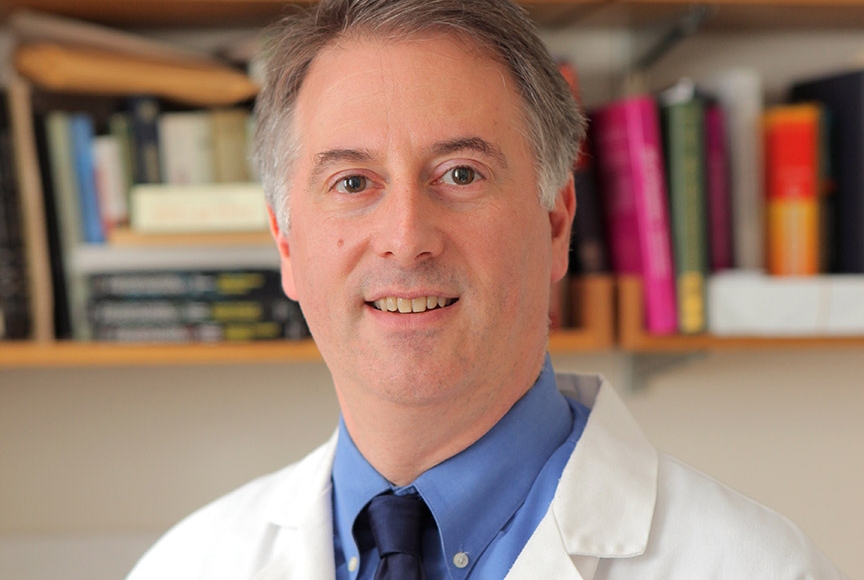
"If further research continues to be positive, we will have, for the first time, a systematic, scientific way to look at the very injured brain, put individual injuries on a continuum of damage, and predict if stimulating this circuit will help restore some brain function," says the study's senior investigator, Dr. Nicholas Schiff, the Jerold B. Katz Professor of Neurology and Neuroscience in the Feil Family Brain and Mind Research Institute and a professor of healthcare policy and research at Weill Cornell.
There are about 300,000 severely brain-injured patients in the United States, many of whom are trapped in a minimally conscious state who may retain some awareness, says Dr. Schiff, who is also a neurologist at NewYork-Presbyterian Hospital/Weill Cornell Medical Center.
Schiff and his colleagues have dubbed the crucial network affected in severe brain injury the mesocircuit.
Centered in the frontal part of the brain, the circuit links the frontal cortex, central thalamus, striatum, and other regions, all of which work to drive attention, alertness, sleep, short-term memory, reward, and motivation, among other functions.
"The central thalamus, as one of the main structures in the mesocircuit, is a hub that is strongly dependent for its activity on other brain structures," Dr. Schiff says. "Therefore, a little bit of damage everywhere has the potential to shut down the mesocircuit."
The researchers tested this hypothesis by measuring if levels of glucose (sugar) metabolism in the mesocircuit of brain-injured patients were lower than in normal brains, which would reflect a loss of function.
The study's lead author, Dr. Esteban Fridman, a post-doctoral associate in neuroscience at the Brain and Mind Research Institute, developed an imaging algorithm and a procedure that allowed him to test mesocircuit metabolism using PET scans, which provide images of biologic activity. He found that gradations of reduced activity within certain mesocircuit structures correlated with the severity of brain injury and behavior, such as whether or not a patient could follow spoken commands.
The findings not only provide supporting evidence for the mesocircuit theory, but implicate three different areas along the circuit that could be targets for drugs that switch those areas back on, Dr. Schiff says. He added that the PET algorithm that Dr. Fridman developed and the findings can be used to assess whether therapies could rescue cognitive capacity in individual brain-injured patients.
"We now have a road map we can follow to assess the potential that brain injury can be reversed, to some degree, in patients," Dr. Schiff says. "This is what all of us who care for these patients are hoping to see evolve further."